Peritoneal dialysis: Open catheter insertion in CAPD - general and visceral surgery
You have not purchased a license - paywall is active: to the product selection
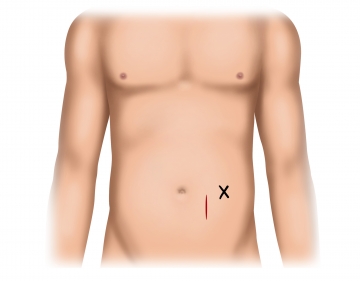
Incising the pararectal skin and exposing the anterior rectus sheath lamina
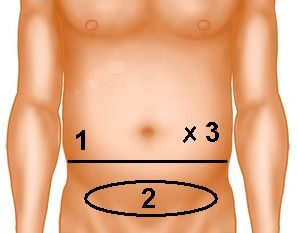
Exposing the posterior rectus sheath lamina and dividing the peritoneum
Incise the anterior lamina of the rectus sheath in a sagittal direction and dissect the rectus muscle in blunt fashion. Open the peritoneum superior to the arcuate line and preplace a peritoneal suture (PDS 3/0) at the inferior pole of the incision.
Tip:
- For better stability, the catheter should be inserted superior to the arcuate line.
- Use a monofilament suture when closing the peritoneum and anchoring the catheter because this helps avoid suture hole laceration.
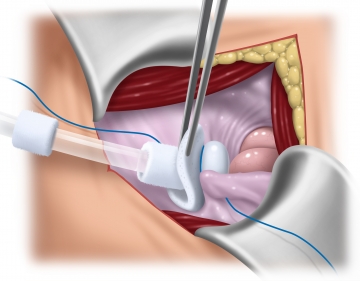
Placing the dialysis catheter and closing the peritoneum
Insert the CAPD catheter into the Douglas pouch with dressing forceps. When closing the peritoneum subsequently with a running suture (PDS 3-0), the latter incorporates the catheter such that the intra-abdominal silicone bead of the catheter adheres to the peritoneum, while the extraperitoneal felt plate rests anterior to the posterior lamina of the rectus sheath. This ensures secure catheter fixation and “watertight” closure of the peritoneum.
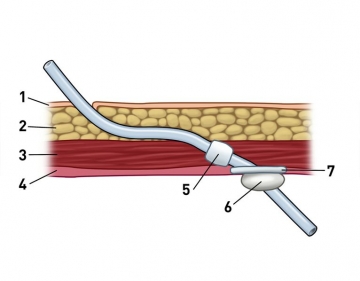
Exiting the dialysis catheter
Figure on right: (1) Skin, (2) subcutaneous tissue, (3) rectus muscle, (4) peritoneum/fascia, (5) felt cuff, (6) silicone bead, (7) felt plate
Mount the free end of the catheter on the tunneling stylet, pull the catheter through the rectus muscle in staggered fashion and let it exit through the skin at the previously marked location. With this maneuver the second felt cuff will rest within the rectus muscle. Mount the titanium adapter.
Tip:
- The submuscular course of the catheter should be smooth avoiding any kinking.
Checking the correct catheter placement by fluoroscopy
Function testing the dialysis catheter
Wound closure, dressing
Single Access
Access to this lecture
for 3 days
€4.99 inclusive VAT

webop-Account Single
full access to all lectures
price per month
for the modul: vascular surgery