Open incisional hernia repair with retromuscular mesh augmentation - general and visceral surgery
You have not purchased a license - paywall is active: to the product selection
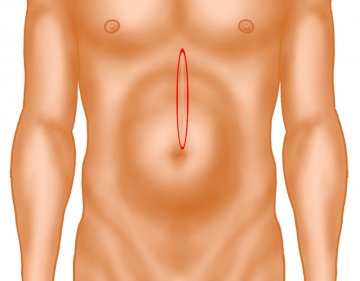
Exzision der Hautnarbe
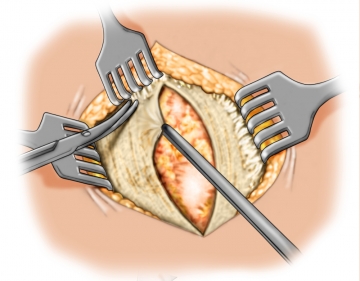
Exposing the fascial defect
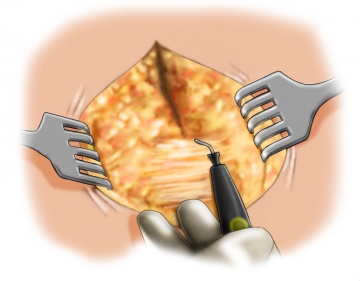
Opening the abdominal cavity
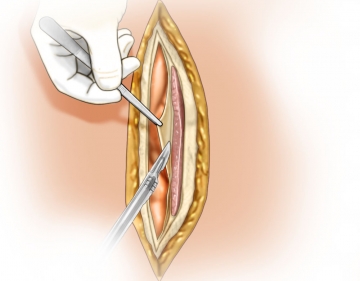
Local adhesiolysis
Local adhesiolysis of abdominal organs in the hernia sac allows better overview and helps avoid iatrogenic bowel lesions when dissecting the tissue for the mesh bed.
Follow this by covering the abdominal cavity with a warm wet laparotomy pad.
Note: Interenteric adhesiolysis should only be performed in case of pertinent complaints
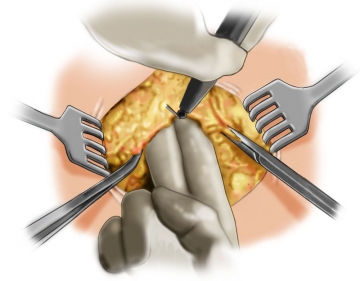
Dissecting the anterior fascia
Incising the rectus sheath
Dissecting the mesh support
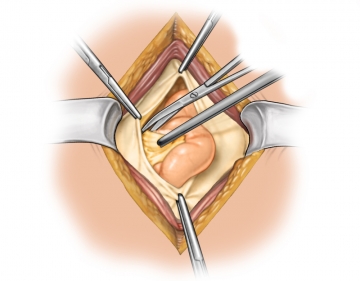
Closing the abdominal cavity
Measuring the mesh bed
Placing and fixating the mesh
Closing the anterior rectus sheath
Fixating the umbilicus and closing the wound in layers
date of update: 10.04.2024
date of publication: 25.04.2009
Single Access
Access to this lecture
for 3 days
€4.99 inclusive VAT

webop-Account Single
full access to all lectures
price per month
for the modul: vascular surgery