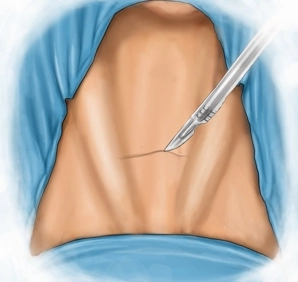
Standard skin incision 2 finger widths (2-3 cm) superior to the suprasternal notch between the bellies of the left and right sternocleidomastoid muscles.
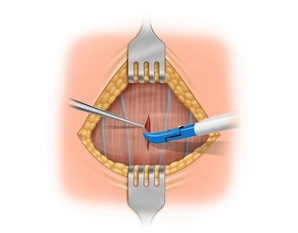
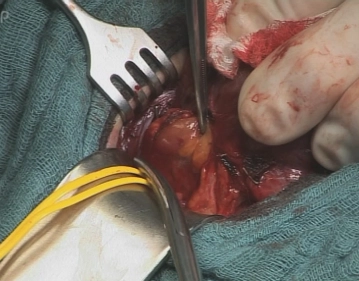
With the Ligasure® divide subcutaneous tissue and platysma down to anterior fascia of the neck.
Expose the avascular plane between platysma and anterior cervical fascia of and free the skin-platysma flap cephalad and caudad.