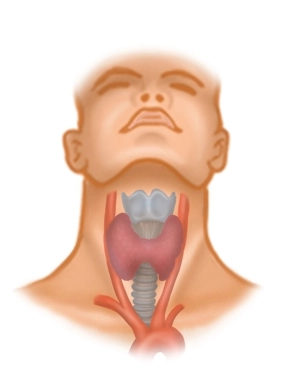
Located between the anterior border of the sternocleidomastoid muscle, the mandible, and the jugular fossa, the anterior triangle of the neck contains the supra- and infrahyoid muscles, vessels, nerves, and the thyroid gland around the hyoid bone. For thyroidectomy, among the infrahyoid muscles, the medially located
• Sternohyoid muscle (sternum → hyoid bone) and beneath it the
• Sternothyroid muscle (sternum → thyroid cartilage of the larynx) as well as more laterally the
• Omohyoid muscle (scapula → intermediate tendon → hyoid bone)
are significant, as they partially cover the thyroid gland and must be retracted intraoperatively.
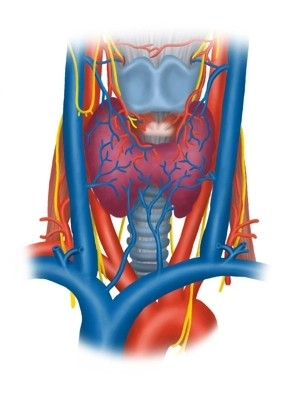
Blood Vessels
The common carotid artery divides at the upper edge of the thyroid cartilage at the level of its carotid sinus (receptors for blood pressure and chemoreceptors for blood gases) into its internal and external branches and runs immediately lateral in the carotid sheath next to the trachea and esophagus cranially. Here it touches the right and left thyroid lobes as a large vessel. The internal jugular vein arises from the sigmoid sinus of the skull, collecting blood from the skull and neck, initially attaching to the internal carotid artery in the carotid sheath, then running further laterally and enclosing the common carotid artery and the vagus nerve (X) laterally.
Nerves
In addition to the vagus nerve and its superior branch to the larynx (superior laryngeal nerve → anterior cricothyroid muscle and mucosa of the upper larynx), the deep cervical ansa (superior and inferior roots, from C1-C3) descends laterally in the thyroid region for the innervation of the three mentioned muscles of the anterior triangle of the neck and the transverse cervical nerve (from C2/3, skin innervation, platysma).
Fascial Layers
In the anterior triangle of the neck, there are several fascial layers under the skin (all belonging to the cervical fascia) that have certain peculiarities:
• The superficial lamina superficialis surrounds all neck structures except the platysma and separately encloses the sternocleidomastoid muscle and dorsally the trapezius muscle (accessory nerve XI),
• the middle lamina pretrachealis surrounds the infrahyoid muscles, and the
• deep lamina prevertebralis runs between the esophagus and spine outside the surgical area.
The thyroid/parathyroid glands and the trachea, as well as the lateral vascular-nerve bundle (carotid artery, internal jugular vein, and vagus nerve), also have their own organ fascias. The arrangement of the cervical fascias results in compartments enclosed by them and spaces (spatium) between them that extend into the mediastinum and represent potential infection pathways.