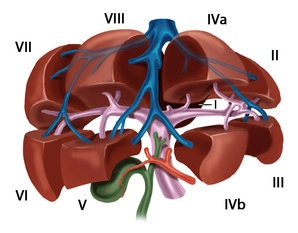
The functional division of the liver is based on the portal branching into individual, independent subunits, the segments.
Usually, the portal vein divides in the hepatic hilum into a right and left main trunk. The boundary of these supply areas lies in the cava-gallbladder line (“Cantlie line”). Through renewed bifurcation of the respective portal vein trunk, an anteromedial as well as a posterolateral trunk arises on the right side for the liver segments V/VIII and VI/VII, respectively. The left main trunk extends transversely to the left and then as the pars umbilicaris anteriorly and ends at the insertion site of the ligamentum teres hepatis in the so-called recessus rex. The left portal main trunk gives off branches for the two left-lateral segments II and III as well as for the median segments IVa and IVb. The caudate lobe occupies a special position, as it can receive strong inflows from the left and also from the right portal vein main trunk.
According to Couinaud, eight portal venous liver segments are distinguished, which, starting with the caudate lobe as segment I, are numbered clockwise:
The liver is traversed in a caudocranial direction by three main venous trunks, namely the right, middle, and left hepatic veins, which divide the liver into a total of four hepatic sectors. The left hepatic vein drains almost exclusively the left-lateral hepatic lobe and usually unites shortly before its entry into the vena cava with the middle hepatic vein, which runs along the cava-gallbladder line. The right hepatic vein runs between the posterolateral and anteromedial segments. The caudate lobe has an independent venous drainage, which consists of multiple small veins emptying dorsally directly into the vena cava, the so-called Spieghel veins.
The portal hila of liver segments II, III, and IV are located extrahepatically and can be relatively easily dissected in the anterior section of the left umbilical fissure. The hila of the right-sided liver segments are located intrahepatically. Exceptions occur occasionally and usually concern segment VI. The anatomy of the hepatic veins is even more variable than that of the portal vein.
Variants
Portal Vein System
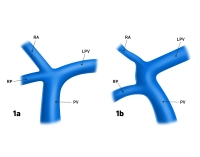
- Anomalies of the portal vein bifurcation almost always affect the right portal vein main trunk
- Portal vein trifurcation: right main trunk is absent, instead there are two branches for the right double segments V/VIII and VI/VII (Fig. 1a); occasionally one of the right branches can also originate from the left portal vein main trunk (Fig.1b)
- Variants of the left portal vein system rarely affect the main trunk, but almost always the division: several small portal vein branches instead of two segmental branches IVa/IVb, occasionally also an additional, intermediate branch between the segmental branches II and III
Fig. 1a and 1b: PV = portal vein, LPV = left portal vein, RA = right anterior portal vein branch, RP = right posterior portal vein branch
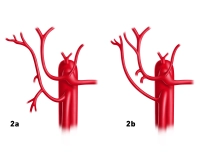
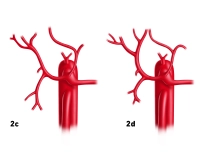
Hepatic Veins
- Variants of the hepatic veins are more common than those of the portal vein system
- Deviations from the hepatic sectors described by Couinaud particularly affect the territories of the right and middle hepatic vein