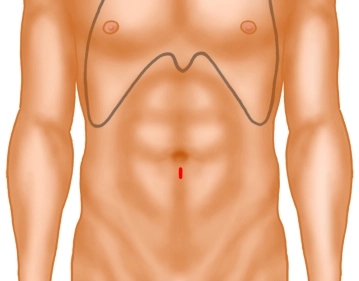
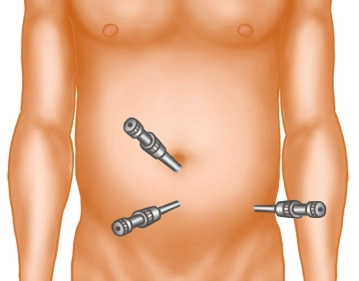
1 cm long skin incision below the navel. Separate the adipose tissue with Langenbeck hooks and expose the fascia or anterior rectus sheath. This is incised with the scalpel on the side to be treated or, in the case of a bilateral hernia as in the example, on the side of the larger hernia, paramedian over a length of approximately 1 cm. The medial edge of the fascia is grasped with a sharp clamp. Using a Langenbeck hook, the medial rectus muscle is lifted anteriorly and laterally, thus exposing the posterior layer of the rectus sheath.
Tip: With a precisely median incision of the fascia, one enters directly into the abdomen and not into the rectus sheath. The fascia must then be closed again and incised further laterally!