After a subumbilical transverse skin incision, the anterior rectus sheath is exposed with two Langenbeck retractors and incised transversely with a scalpel. The medial edge of the rectus muscle is loaded onto the retractors and a dissection balloon is introduced. This balloon glides on the posterior layer of the rectus sheath up to the pubic bone. Under visual control with the 0° optics, the expansion of the extraperitoneal space allows for blunt dissection and clear identification of the key structures: pubic bone, rectus muscle, and epigastric vessels. The balloon is removed and the incised anterior rectus sheath is reinforced with braided, absorbable sutures of size 0.
-
Access to the Extraperitoneal Space
-
Insertion of the Optic and First Working Trocar
Soundsettings Now a blunt gas-tight 10 mm trocar with a fixation device is inserted and secured with the pre-placed sutures. Usually, a working pressure of 7 mmHg is sufficient to adequately expand the extraperitoneal space. A 5 mm trocar is inserted in the midline at least 5 cm above the pubis.
Tip:
A non-conductive, short 5 mm threaded trocar is recommended. -
Preparation of the Extraperitoneal Space with Insertion of the Third Trocar
![Preparation of the Extraperitoneal Space with Insertion of the Third Trocar]()
Soundsettings With Overholt and optics, the medial preperitoneal space is initially expanded, crossing the midline. The dissection proceeds laterally from here, with a large medial hernia clearly visible. The lateral preparation along the transversus abdominis muscle is continued up to the level of the navel. At this level in the anterior axillary line, the third trocar is now inserted, optionally as a 5mm or, as in the example, a 10mm trocar.
Remarks:
- Through this position of the second working trocar, good triangulation can be achieved.
- During lateral preparation, especially when using electrocautery, the course of the lateral femoral cutaneous nerve must be observed.
-
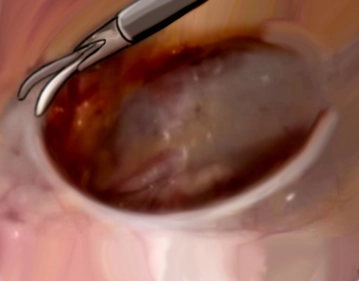
Detachment of the Hernia Sac from the Spermatic Cord Structures
![Detachment of the Hernia Sac from the Spermatic Cord Structures]()
Soundsettings After all trocars are inserted, the camera operator changes position and now stands behind the surgeon. The table is tilted towards the team's side, and a head-down tilt of 10° is usually helpful. A large direct hernia sac is now detached from the spermatic cord under identification of the ductus deferens and the vessels, and prepared sufficiently cranially to allow optimal mesh placement later.
-
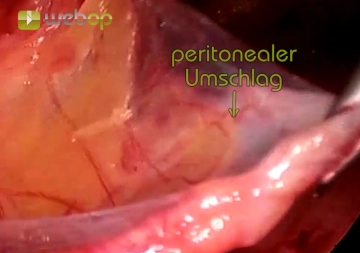
Dissection of the Peritoneum (Parietalization)
![Dissection of the Peritoneum (Parietalization)]()
Soundsettings If the linea arcuata extends far down, as in the example, it should be incised laterally. The final act of dissection is then the separation of the peritoneum from the spermatic cord structures or the fascia spermatica up to above the middle of the psoas towards the abdomen. All even the smallest fibrous connections between the peritoneum and retroperitoneum must be severed. Here, the inguinal nerves are now exposed, laterally from the psoas muscle the lateral femoral cutaneous nerve, medially the genitofemoral nerve.
A preperitoneal lipoma accompanying the spermatic cord structures should be highly mobilized or res
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$86.33/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$172.70 / yearly payment