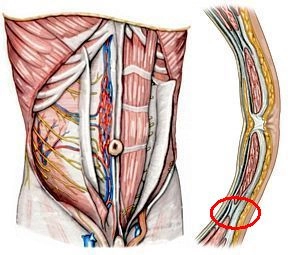
1. Anterior Abdominal Muscles
M. rectus abdominis: straight abdominal muscle within the rectus sheath with 3-4 tendinous intersections (Intersectiones tendineae), which are fused with the anterior layer of the rectus sheath.
M. pyramidalis: originates at the superior pubic ramus and radiates into the linea alba, located ventrally to the M. rectus abdominis in its own sheath in the anterior layer of the rectus sheath.
2. Layer Structure of the Anterior Abdominal Wall
Rectus sheath: envelops the M. rectus abdominis; above the midpoint between the navel and symphysis, a distinction is made between an anterior and a posterior layer; the posterior layer ends here in the form of the linea arcuata; above this linea, the M. obliquus externus abdominis radiates into the anterior layer of the rectus sheath, the M. obliquus internus abdominis into both the anterior and posterior layers, and the M. transversus abdominis into the posterior layer.
Linea semilunaris: transition zone between the aponeuroses of the lateral abdominal muscles and the lateral edge of the rectus sheath.
Linea alba: approximately 1 cm wide firm connective tissue strip between the right and left rectus sheath, extending from the sternum to the symphysis.
Fascia transversalis: above the linea arcuata, it covers the posterior layer of the rectus sheath internally, below the linea it lies directly on the M. rectus abdominis.
3. Internal Relief of the Abdominal Wall
Plica umbilicalis mediana: median peritoneal fold running from the navel to the bladder, within the fold is the Lig. umbilicale medianum (connective tissue strand = urachus remnant).
Plica umbilicalis medialis: paired peritoneal fold, contains on both sides the Lig. umbilicale mediale = obliterated remnant of the bilateral umbilical artery, A. umbilicalis.
Plica umbilicalis lateralis: paired peritoneal fold, beneath it lies on both sides the A. epigastrica inferior with two accompanying veins each.
4. Conduits
a) Arteries
A. epigastrica superior: continuation of the A. thoracica interna, anastomoses at the level of the navel with the A. epigastrica inferior.
A. epigastrica inferior: arises from the A. iliaca externa and runs like the aforementioned artery on the dorsal surface of the M. rectus abdominis in the rectus sheath.
A. epigastrica superficialis: originates from the A. femoralis and distributes in the subcutaneous tissue of the anterior abdominal wall after crossing the inguinal ligament.
Aa. intercostales posteriores VI – XI and A. subcostalis: originate from the thoracic aorta; their terminal branches run obliquely downward between the M. obliquus internus abdominis and M. transversus abdominis and extend from laterally to the rectus sheath, where they anastomose with A. epigastrica superior et inferior.
b) Veins
Vv. epigastricae superiores: accompany the artery of the same name; anastomose with branches of the V. epigastrica inferior and drain into the Vv. thoracicae internae.
V. epigastrica inferior: branches into accompanying veins of the A. epigastrica inferior and drains into the V. iliaca externa.
V. epigastrica superficialis: runs parallel to the artery of the same name (see above).
c) Lymphatic Vessels
Superficial lymphatic vessels: above the navel, they run to the axillary lymph nodes (Nodi lymphatici axillaris), below to the inguinal lymph nodes, Nodi lymphatici inguinales.
Deep lymphatic vessels: usually run parallel with the blood vessels; reach the Nodi lymphatici parasternales, lumbales, and iliaci externi.
d) Nerves
Nn. intercostales VI – XII: as Rr. ventrales of the Nn. thoracici VI – XII; they enter the abdominal wall behind the costal cartilages between the M. obliquus internus abdominis and M. transversus abdominis; motor branches supply the anterior and lateral abdominal muscles, the sensory branches the abdominal skin.
N. iliohypogastricus, N. ilioinguinalis, and N. genitofemoralis: participate in the motor and sensory innervation of the lower abdominal region and genitalia.