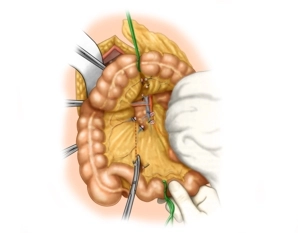
As an example, the suture is demonstrated in a right-sided hemicolectomy. An ileotransversostomy is planned. Owing to the long mesenteries, the intestine can be rotated here; therefore, the anterior wall will be sutured first, and after rotating the intestine this will be followed by the posterior wall.
-
Selecting the intestinal loop
-
Dissecting the intestinal wall
First, dissect free both intestinal walls at the planned anastomosis. Limit skeletonization of the intestinal wall to less than 1.5 cm for the small intestine and no more than 0.5-1 cm for the large bowel. Always check for a healthy, grayish-red color of the intestinal tissue, bleeding wound edges, and palpable or visible arterial pulses in the intestinal section to be sutured.
-
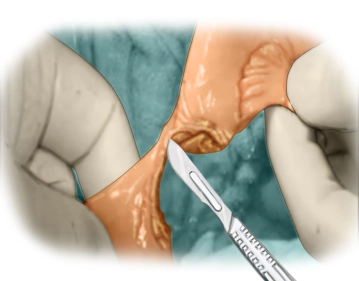
Resecting the intestine
Block the intestine with intestinal clamps. By transecting the intestine with the scalpel perfusion of the intestinal wall will not be jeopardized.
Note: The ileum is resected at an oblique angle to account for the bigger lumen of the transverse colon; if necessary, extend the ileum length of the anastomosis by slitting the ileum along its antimesenteric aspect.
-
Intestinal suture 1 (placing the stay sutures)
Principle: Single-layer, extramucosal continuous full-thickness suture with two absorbable threads
Material: Synthetic absorbable suture, monofilament or braided, size 3-0 or 4-0First, place one suture each on the mesenteric and antimesenteric aspect as an orientation and stay suture. This will half each intestinal lumen and assign it to its corresponding counterpart Tie the ends of the antimesenteric stay suture. One end of this tied stay suture in turn serves as another stay suture, while the anterior wall of the anastomosis is sutured with the other end.
When placing the suture, take care not to include the mucosa (extramucosal suture), but stitch unde
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
€44.50 / yearly payment
general and visceral surgery
Unlock all courses in this module.
€149.00 / yearly payment