The stomach is – formally speaking – a bulge of the digestive tract that lies between the esophagus and the intestine and has the task of storing and mixing food. This muscular hollow organ forms acidic gastric juice (mucus and HCl) and enzymes that pre-digest some components of the food, in order to then pass the food pulp portionwise into the small intestine.
The stomach is usually located in the left and middle upper abdomen directly under the diaphragm. The position, size, and shape of the stomach vary greatly from person to person and depending on age, filling state, and body position. When moderately filled, the stomach is on average 25-30 cm long and has a storage capacity of 1.5 and in extreme cases even up to 2.5 liters.
The stomach is attached and stabilized in the abdominal cavity by ligaments that, among other things, extend to the liver and spleen. It forms with its convex side the greater curvature of the stomach (greater curvature of the stomach / Curvatura major) and with the concave side the lesser curvature of the stomach (lesser curvature of the stomach / Curvatura minor). Its anterior wall is called Paries anterior, its posterior wall Paries posterior.
The stomach lies intraperitoneally and thus shows a covering of serosa, only the dorsal cardia is free of serosa. The embryonic mesogastria reach through the stomach rotation from their formerly sagittal position into a frontal one: The lesser omentum extends from the lesser curvature to the porta hepatis, the greater omentum spreads from the greater curvature to the transverse colon, the spleen, and the diaphragm.
One can divide the stomach into various sections:
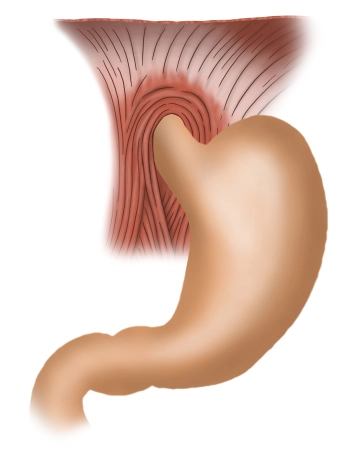
- Stomach entrance / Cardia / Ostium cardiacum:
The upper stomach opening is an area of 1-2 cm where the esophagus opens into the stomach. Here is the sharp transition from the esophageal mucosa to the gastric mucosa, which can usually be easily recognized with the endoscope. - Stomach fundus / Fundus gastricus:
Above the stomach entrance, the fundus bulges upwards, also called "stomach dome" or Fornix gastricus. The fundus is usually filled with air that is involuntarily swallowed during eating. In an upright person, the fundus forms the highest point of the stomach, so that in the X-ray image, the collected air is recognizable as a "gastric bubble". Opposite the stomach entrance, the fundus is delimited by a sharp fold (Incisura cardialis). - Stomach body / Corpus gastricum:
The main part of the stomach is formed by the stomach body. Here lie deep longitudinal mucosal folds (Plicae gastricae), which extend from the stomach entrance to the pylorus and are also referred to as the "gastric street". - Pylorus / Pars pylorica:
This section begins with the expanded Antrum pyloricum, followed by the pyloric canal (Canalis pyloricus) and ends with the actual pylorus (Pylorus). Here lies the pyloric sphincter (M. sphincter pylori), which is formed by a strong annular muscle layer and closes the lower stomach opening (Ostium pyloricum). The pylorus closes the stomach outlet and periodically allows some food pulp (chyme) to pass into the subsequent duodenum.