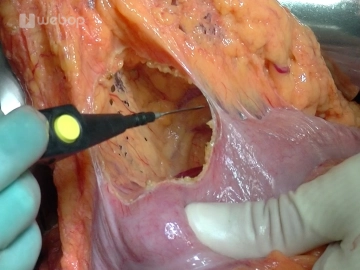
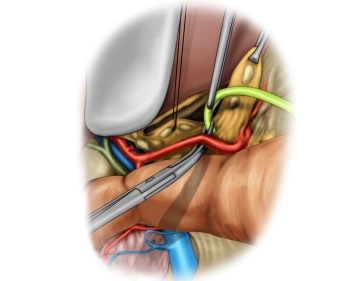
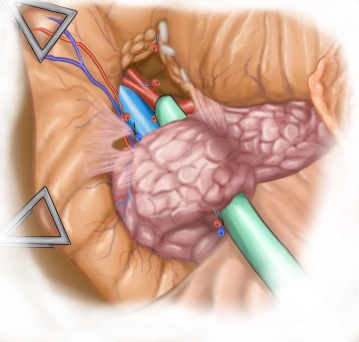
Fashion the pancreatojejunostomy in two rows with the duct anastomosed end-to-side. To this end, mobilize the pancreas far enough to the left of the superior mesenteric vein and probe the duct. First, at the pancreas preplace double-armed full-thickness interrupted mattress sutures through the jejunal limb serosa.
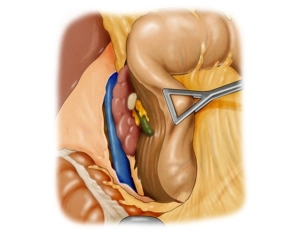
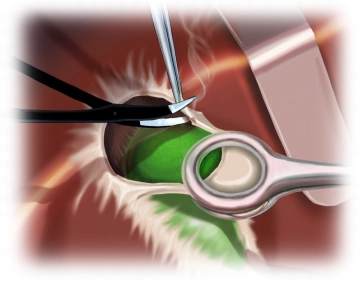
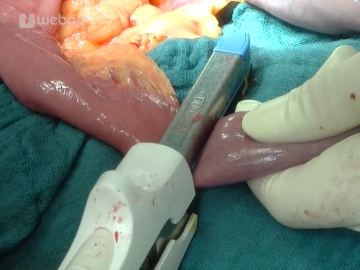
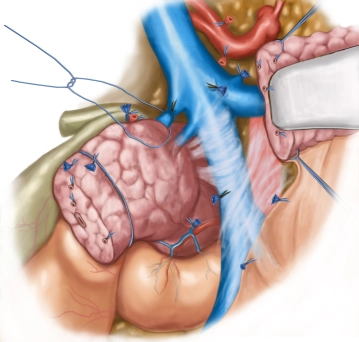
After punctiform opening of the jejunum, pull up the mucosa with three everting interrupted sutures. First, preplace the inner suture row (duct-to-mucosa) with double-armed sutures. The full-thickness sutures encompass the entire wall, including the pancreatic duct and corresponding jejunum. The suture direction is from the inside out, with the knots later located on the outside. Then tighten the preplaced transpancreatc interrupted sutures, approximating the pancreatic stump to the jejunum. Next, tie the knots of these sutures but do not off the ends of the thread.
Tying the duct-to-mucosa knots completes suture of the posterior wall.
Note:
The main emphasis when fashioning a pancreatic anastomosis should be on tension-free approximation and good perfusion, while avoiding obstruction of the pancreatic duct.