Incisional hernia is a clinical diagnosis and easily recognized with the patient standing. Also, examine the patient supine when he/she is relaxed. In most reducible incisional hernias, the margin of the fascia is easily palpated Asking the patient to elevate the upper trunk allows good assessment of the surrounding muscles and the size of the fascial defect.
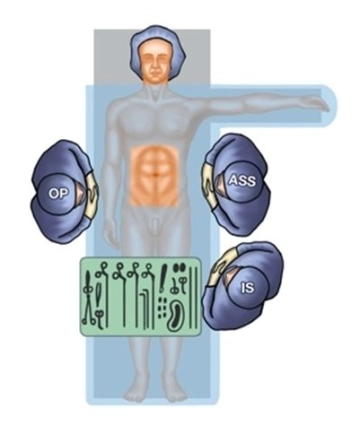
Apart from measuring the size of the fascial defect and content of the hernia sac, ultrasonography provides a good anatomical view of the abdominal wall. Important questions are: Location and size of the abdominal muscles, such as the rectus abdominis in median incisional hernias and the lateral abdominal muscles in incisional hernias outside of the rectus sheath.
In previously repaired incisional hernia, the pertinent OR not would be helpful, particularly if the patient had already undergone mesh repair. Apart from the precise surgical technique employed (extra-/intraperitoneal mesh placement, augmentation or bridging of the fascial defect), the type of mesh material would also be important.
CT and/or MRI studies are not mandatory. In our experience, these studies have their place in gigantic incisional hernias because there they permit better assessment of the abdominal wall.
Depending on the size of the finding and patient morbidity, preoperative diagnostic lung function testing is important to prevent, as much as possible, postoperative respiratory complications.