After the start of the operation (establishment of the capnoperitoneum, placement of the working trocars, inspection of the abdominal cavity), the exposure of the angle of His follows.
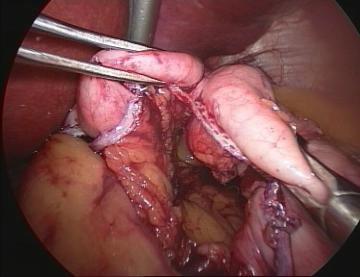
Subsequently, the formation of the gastric pouch begins in the area of the lesser curvature 2 cm below the esophagogastric junction. The left gastric artery supplies the gastric pouch and is taken into account to avoid bleeding complications and to ensure the blood supply of the pouch. The transection of the stomach is initially performed in a horizontal direction with linear stapling devices (staple height 3.5 mm).
The dissection is then continued in a triangular shape towards the left diaphragmatic crus. The left crus of the diaphragm serves as the anatomical target line.
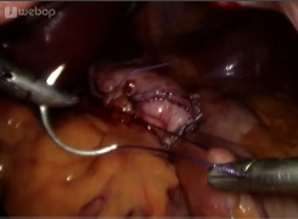
The fundus should be completely severed to exclude the production site of the entero hormone ghrelin from the food passage and to avoid later dilatation.
Finally, sufficient hemostasis at the staple line should be performed with ultrasound.