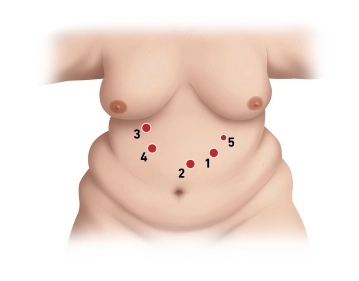
Position the camera trocar in the left epigastrium, approximately 2-3 fingerbreadths caudal to the left costal arch in the midclavicular line.
Access is by means through an optical trocar (12 mm Xcel trocar) under camera view. During insertion, ensure that the individual tissue layers can be viewed. During insertion, optical trocars ensure a clear view of the individual tissue layers. Place the additional trocars under camera view and after placement the patient into the anti-Trendelenburg position.
Then place three more 12 mm trocars in the following order: First trocar about 1.5 hand widths inferior to the xiphoid process paramedian on the left (far supraumbilical) and the second trocar roughly in the midclavicular line immediately at the right costal arch, guiding the trocar tip in the direction of the patient's left leg. Finally insert the third 12 mm trocar about one hand’s width caudal to the right costal arch medial to the midclavicular line in the right upper quadrant. Then and finally insert an additional 5 mm trocar at the left costal arch somewhat cranial to the first 12 mm trocar.
Note: A liver retractor is needed only for extremely large livers, which is the case in less than 5% of patients.