Appendectomy is the most common abdominal surgery worldwide. The lifetime risk of appendectomy is 7-8%.
This paradigm in the treatment concept of acute appendicitis is currently causing intense discussions and is being questioned since conservative treatment models have been published and have found access to public opinion formation.
Currently, the data is insufficient to recognize an advantage of conservative therapy, especially in the uncomplicated form, and therefore no recommendation for the conservative therapy of appendicitis can be made. Recommendations for the treatment of acute appendicitis have been developed based on evidence both in the journal Chirurg (recommendations of an expert group against the background of current literature: Andric et al. Chirurg 2020; 91:700-711) and in the Deutsches Ärzteblatt (Téoule et al. Dtsch Arztebl Int 2020; 117: 764-74).
An acute appendicitis can be classified into uncomplicated and complicated appendicitis depending on the degree of severity. According to the EAES (European Association of Endoscopic Surgery), uncomplicated appendicitis is an inflammation of the appendix without evidence of gangrene, surrounding phlegmon, free purulent fluid, or abscess.
The classification of acute appendicitis into uncomplicated or complicated form should be made pre-therapeutically to select appropriate therapy.
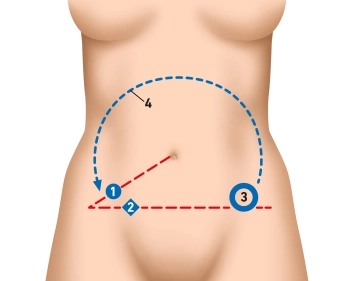
For many years, the open access route via the right lower abdominal incision was considered the standard procedure. Today, a laparoscopic appendectomy is routinely performed in Germany. However, the open access route still has its justification. Both surgical approaches are legitimate worldwide.
An incidental appendectomy in the absence of contraindication is possible because, despite a macroscopically inconspicuous appendix, histologically appendicitis or other pathologies such as endometriosis, neoplasia, obstruction by appendicoliths, or parasites may be present.
Uncomplicated appendicitis can be treated conservatively under appropriate conditions. However, a meta-analysis published in 2019 (Prechal et al.: Antibiotic therapy for acute uncomplicated appendicitis: a systematic review and meta-analysis. Int J Colorectal Dis 2019) shows that up to 37% of originally conservatively treated adult patients undergo appendectomy within a year.
Risk factors for conservative therapy failure and increased morbidity include the presence of an appendicolith, obesity, age > 65 years, immunosuppression, acquired immune deficiencies, and pregnancy.
In case of failure of non-operative therapy (persistence or progression of symptoms; approx. 14%), urgent surgery must be performed. This often results in a complicated, technically demanding surgical situation.
Complicated appendicitis is a serious condition. In the case of free perforation, immediate surgery is required.
In the case of periappendicular phlegmon or perityphlitic abscess, the current data does not allow a safe recommendation for the timing of surgery. A prompt appendectomy is generally recommended, especially in patients with risk factors, while macro abscess and inflammatory conglomerate tumor are more likely to be treated interventionally and/or with antibiotics.
If an appendix/residual appendix is sonographically detected after 6-8 weeks, an interval appendectomy should be performed.
According to current literature (Li et al.: Effect of delay to operation on outcomes in patients with acute appendicitis: a systematic review and meta-analysis. J Gastrointest Surg 2019; van Dijk et al.: Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br J Surg 2018; Cameron et al.: Time to appendectomy for acute appendicitis: A systematic review. J Pediatr Surg 2018; 53: 396–405), an appendectomy under antibiotic therapy in imaging-suspected uncomplicated cases can be delayed 12-24 hours from diagnosis without increasing the perforation rate. Exceptions exist for patients over 65 years or with relevant comorbidities, especially immunosuppression and immune deficiency, where early surgery should be performed and a time interval of 12 hours should not be exceeded. The same applies to children and adolescents.
In pregnant women, due to the risk of miscarriage, urgent appendectomy should be performed. An appendectomy can be performed without problems in any trimester.
If the appendix is macroscopically inconspicuous intraoperatively and there is no differential diagnosis, an appendectomy should be performed, as in 29% of these cases histologically appendicitis is diagnosed. If another diagnosis is made intraoperatively, removal of the appendix can be omitted.
Tumors of the appendix as a histopathological incidental finding:
In appendectomy specimens examined by pathologists, tumors are found as incidental findings in up to 2% of specimens in histopathological processing. These tumors of the appendix can be classified according to the WHO classification into the two main groups of neuroendocrine tumors (NET) and mucinous neoplasms.
The neuroendocrine tumors of the appendix, the so-called appendiceal carcinoids, are rare histological incidental findings almost exclusively observed postoperatively after appendectomy. Most are located at the tip of the appendix, are smaller than 2 cm, and do not metastasize. Therefore, resection is rarely required. The following conditions necessitate a secondary right hemicolectomy with mesenteric lymphadenectomy: primary tumor > 2 cm, mesoappendix infiltration, goblet cell carcinoid, intermediate or high-grade differentiation, R1 appendectomy.
The mucinous neoplasms can be subclassified into invasive mucinous adenocarcinoma and the expansively growing LAMN (low-grade mucinous neoplasms), which are considered precursors of PMP (Pseudomyxoma peritonei).
These mucus-producing tumors of the appendix lumen can rupture over time and lead to seeding in the abdominal cavity.
There are no clear therapeutic regimens in the literature for the incidental finding of a LAMN. Therapy must consider the risk of potential development of PMP and weigh it against the morbidity and mortality of the therapy.
Mc Donald et al. classify LAMN into 2 types, with the presence of mucus or herniation of mucus in the appendix wall, perforation of the appendix wall, or detection of mucus outside the appendix without evidence of perforation being the discriminating criteria.
This classification is the basis for the therapeutic decision in most HIPEC centers.
Only LAMN Type 1 seems to be adequately treated with an R0 appendectomy. For LAMN Type 1 with R1 resection and all LAMN Type 2 tumors, prophylactic HIPEC (Hyperthermic Intraperitoneal Chemotherapy) with local peritonectomy is recommended, with additional resection of the resection margins in the R1 situation. Local peritonectomy in the lower abdomen and HIPEC can be performed laparoscopically.
Invasive mucinous appendiceal carcinoma requires an oncological hemicolectomy, and therapeutic (+ Cytoreductive Surgery (CRS)) or prophylactic HIPEC is recommended.