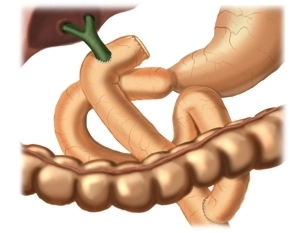
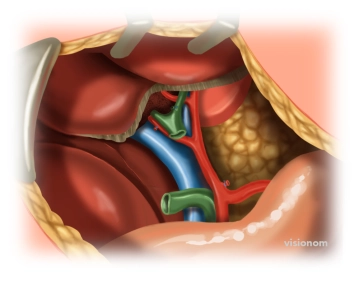
The gold standard in bilioenteric anastomosis is retrocolic end-to-side Roux-en-Y hepaticojejunostomy with a segment of the proximal jejunum.
Here, the preferred bilioenteric anastomosis is established proximal to the cystic duct and about 2-3 cm distal to the union of the hepatic ducts.
- The opening of the anastomosis should be as wide as possible (if the common hepatic duct is too small it may be enlarged with the Hepp-Couinaud technique)
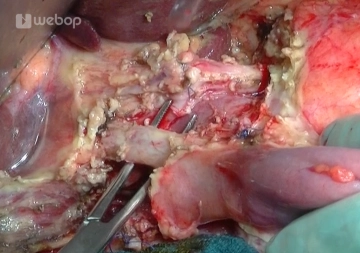
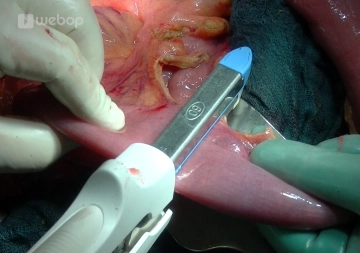
- The single row of interrupted suture encompassing all layers should be leak-roof from the beginning and
- precisely adapt the mucosa of the hepatic duct to that of the jejunum.