The stomach is, formally speaking, a dilation of the digestive tract located between the esophagus and the intestine, tasked with storing and mixing food. This muscular hollow organ produces acidic gastric juice (mucus and HCl) and enzymes that partially digest some components of the food, subsequently transferring the chyme in portions to the small intestine.
The stomach is usually located in the left and middle upper abdomen directly beneath the diaphragm. The position, size, and shape of the stomach vary greatly from person to person and depending on age, state of fullness, and body position. When moderately filled, the stomach is on average 25-30 cm long and has a storage capacity of 1.5 liters, and in extreme cases, up to 2.5 liters.
The stomach is anchored and stabilized in the abdominal cavity by ligaments that extend to the liver and spleen, among others. It forms the greater curvature (Curvatura major) with its convex side and the lesser curvature (Curvatura minor) with its concave side. Its anterior wall is referred to as Paries anterior, and its posterior wall as Paries posterior.
The stomach is intraperitoneal and thus covered by serosa, with only the dorsal cardia free of serosa. The embryonic mesogastria move from their original sagittal position to a frontal one due to the rotation of the stomach: The lesser omentum extends from the lesser curvature to the hepatic portal, while the greater omentum spreads from the greater curvature to the transverse colon, spleen, and diaphragm.
The stomach can be divided into different sections:
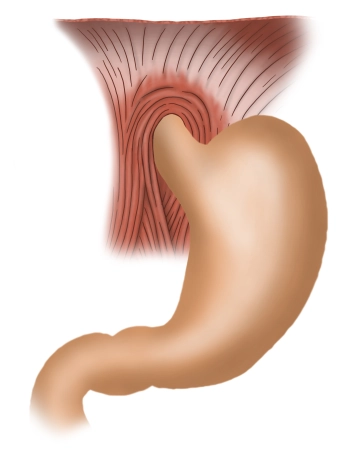
- Cardia / Ostium cardiacum:
The upper gastric mouth is an area of 1-2 cm where the esophagus opens into the stomach. Here, the sharp transition from the esophageal mucosa to the gastric mucosa can usually be well recognized with an endoscope. - Fundus gastricus:
Above the gastric entrance, the fundus arches upward, also known as the "gastric dome" or Fornix gastricus. The fundus is typically filled with air that is involuntarily swallowed during eating. In an upright person, the fundus forms the highest point of the stomach, so in an X-ray, the collected air appears as a "gastric bubble." Opposite the gastric entrance, the fundus is demarcated by a sharp fold (Incisura cardialis). - Corpus gastricum:
The main part of the stomach is formed by the gastric body. Here, deep longitudinal folds of the mucosa (Plicae gastricae) extend from the gastric entrance to the pylorus and are also referred to as the "gastric street." - Pars pylorica:
This section begins with the expanded antrum pyloricum, followed by the pyloric canal (Canalis pyloricus), and ends with the actual pylorus. Here lies the pyloric sphincter muscle (M. sphincter pylori), formed by a strong circular muscle layer, which closes the lower gastric mouth (Ostium pyloricum). The pylorus seals the gastric outlet and periodically allows some chyme to pass into the subsequent duodenum.