According to the guidelines of the EHS and AHS, the laparoscopic IPOM technique is recommended for larger primary and secondary abdominal wall hernias and in patients with an increased risk of wound complications. This particularly applies to patients with obesity (BMI >_ 30) and patients with a defect size greater than 4 cm. However, the defect should not exceed a size of 8 - 10 cm.
The laparoscopic intraperitoneal mesh implantation currently represents the most common endoscopic, minimally invasive technique for the treatment of abdominal hernias worldwide. In Germany, however, there is a decline in this method due to fear of adhesiogenicity with the formation of prosthetic-intestinal fistulas despite improved meshes regarding their coating. Other reasons include an increased rate of acute and chronic postoperative pain, presumably due to mesh fixation on the inner abdominal wall. Additionally, the method is expensive due to significant material costs. Nevertheless, it is an important alternative technique.
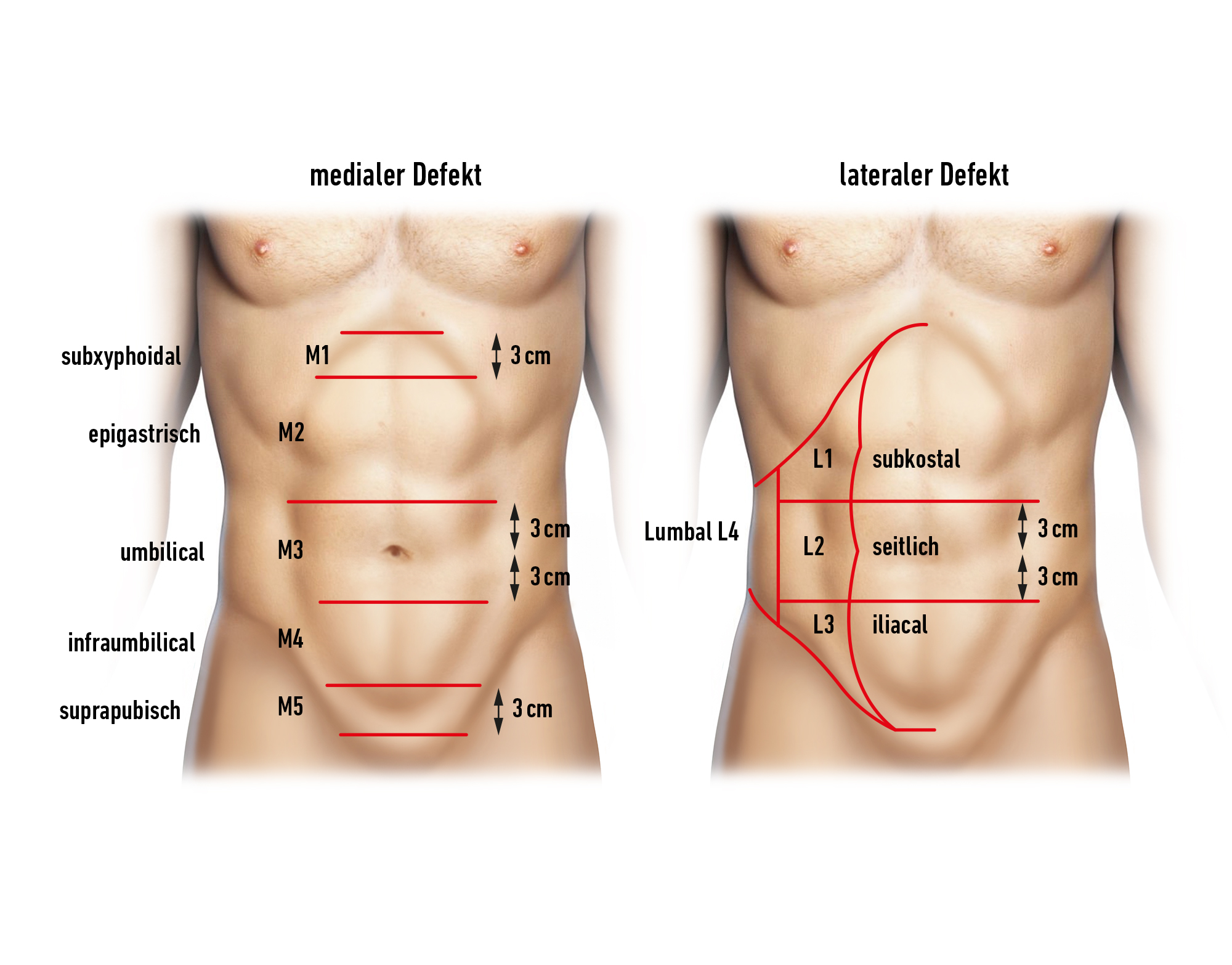
Secondary Abdominal Wall Hernias
Incisional hernia is the most common complication after laparotomy with a prevalence between 3 and 40%, regardless of the abdominal wall closure chosen.
Risk factors for the development of incisional hernias:
BMI >_ 25, male gender, recurrent incision, malignant disease, wound contamination, open surgery, COPD, positive family history.
When determining the indication, the previous surgery should be at least 6 months prior.
Closure of the Hernial Orifice:
There are studies recommending an additional closure of the hernial orifice in IPOM to reduce the rate of recurrences, seroma formation, and pseudo-recurrences. For a small defect (< 3 cm), a direct closure of the defect is performed, and for larger defects, a so-called LIRA (intracorporeal rectus aponeuroplasty) with a knotless suture is used. In a recent study (Pizza F et al 2023), the superiority of hernial orifice closure could not be confirmed.