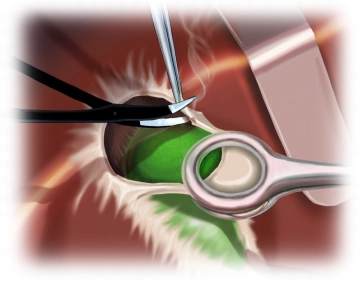
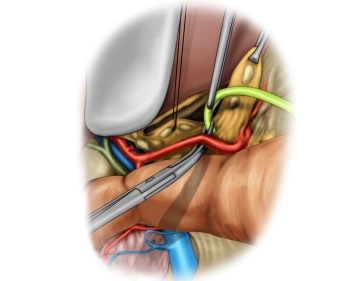
Dissection of the hepatoduodenal ligament includes exposure of the common hepatic artery, proper hepatic artery, and gastroduodenal artery, portal vein, and common bile duct.
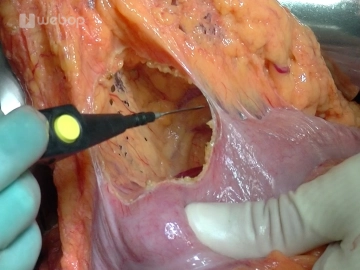
The case presented here has an anatomical variant of the blood supply to the liver. An atypical right hepatic artery from the superior mesenteric artery crosses the common bile duct posteriorly.
In this case, perform the lymphadenectomy along the left hepatic artery in a central direction towards the celiac trunk, exposing the bifurcation of the gastroduodenal artery.
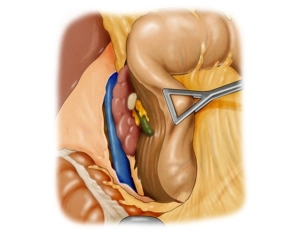
Begin mobilizing the pylorus by dividing the right gastric artery between ligatures.
Before this, complete ligament dissection by exposing the suprapancreatic portal vein until posterior to the pancreas.