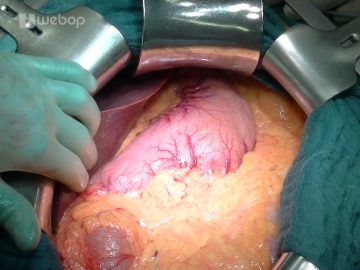
Open the abdomen through a bucket-handle incision about 3-4 fingers below the costal arches with transection of skin, subcutaneous tissue, anterior fascial lamina, rectus muscle and posterior fascial lamina/peritoneum. Divide the round ligament of the liver between clamps and secure the stumps with suture ligatures (Vicryl® 2-0). Free the falciform ligament with monopolar electrocautery far over the anterior aspect of the liver. After draping the margins of the incision with damp lap towels install the retractor system comprising a frame and a cable winch system such as the Ulrich retractor. This is followed by systematic exploration of the abdominal cavity: Liver (metastases?), stomach (tumor? position of gastric tube), small intestine (adhesions? peritoneal carcinomatosis?), large bowel (tumor?), greater omentum (adhesions? carcinomatosis of peritoneal cavity?)
-
Bucket-handle incision
-
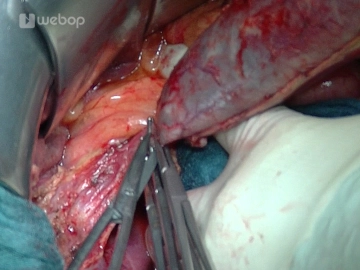
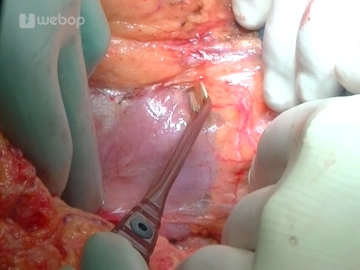
Antegrade cholecystectomy
![Antegrade cholecystectomy]()
Soundsettings The resection phase starts with the antegrade cholecystectomy: After clamping the fundus of the gallbladder release it from the liver bed using bipolar forceps and scissors. Expose the cystic duct and cystic artery, and after clamping each with an Overholt forceps, divide them and secure each central remnant with a suture ligature (Prolene® 3-0). Once the gallbladder has been taken down and handed over for histology, take a swab of the bile secretion for microbiology.
-
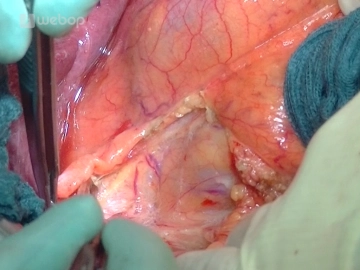
Mobilizing the hepatic flexure/Kocher maneuver
![Mobilizing the hepatic flexure/Kocher maneuver]()
Soundsettings Mobilize the right colic flexure by incising the peritoneal reflection lateral to the ascending colon and carry the incision around the hepatic flexure. Gentle traction on the colon will tauten the avascular tissue plane posterior to the colon, and the mesocolon may be released from the retroperitoneal space, anterior aspect of the duodenum and the head of the pancreas.
Mobilize the duodenum with the Kocher maneuver: Pull the mobilized colon section over to the left, and after incising along the outer margin of the duodenum with bipolar forceps and dissecting scissors release the duodenum together with the head of the pancreas from its retroperitoneal attachments. Continue mobilizing the head of the pancreas across the aortic plane up to the ligament of Treitz so that the head of the pancreas can be completely enclosed and palpated from posterior (tumor size? consistency?)
-
Opening the lesser sac
![Opening the lesser sac]()
Soundsettings Enter the lesser sac by freeing the greater omentum from the hepatic flexure to the left third of the transverse colon. Although the lesser sac displays minor adhesions, it can be easily freed and exposed with the bipolar forceps. This allows pancreatic exploration on the left side as well.
-
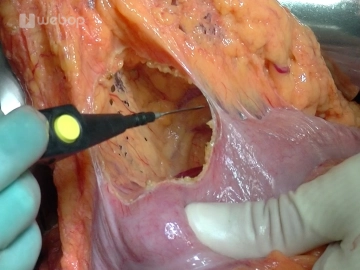
Exposing the inferior aspect of the pancreas and the mesenterico-portalvenous vascular axis
![Exposing the inferior aspect of the pancreas and the mesenterico-portalvenous vascular axis]()
Soundsettings Continue the dissection along the inferior aspect of the pancreas by exposing the superior mesenteric and portal vein. To this end, divide the veins of the pancreatic head with the LigaSure® or between suture ligatures (Prolene® 4-0 or 5-0). Starting in the plane of the superior mesenteric / portal vein now tunnel the pancreas from inferior and place stay sutures at its inferior aspect to the left and right of the portal vein.
Caution: Bleeding from the portal vein! - put as little traction on the tissue as possible!
After opening the lesser omentum and exposing the common hepatic artery at the superior aspect of t
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$87.56/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$175.10 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.