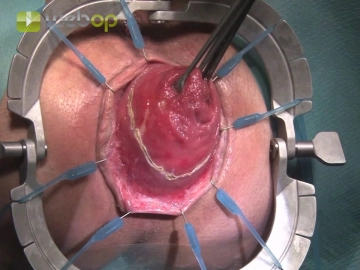
After completely exposing the external prolapse attach the Lone Star retractor and expose the dentate line. Then a circular incision of the outer duplication of the rectal wall 1-2 cm above the dentate line is made under gentle traction at the tip of the prolapse with Allis clamps, so that the anastomosis is later proximal to the puborectal muscle.
-
Inserting the anal retractor and incising the rectal wall
-
Transect the outer duplication of the rectal wall
![Transect the outer duplication of the rectal wall]()
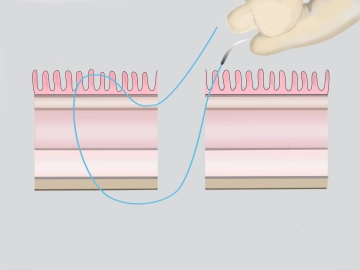
Soundsettings Step by step, transect the rectal wall with bipolar scissors. At each exposed part of this incision, grasp the caudal rectal wall and place Gambee sutures without tying them.
Note: Make the first full-thickness stitch of the absorbable multifilament suture from the submucosa to the inside and the return stitch from the inside to the outside. Put tension on the ends of the suture to open up the anal ring in circular fashion.
The herniated Douglas pouch presents on the anterior circumference of the inner intestinal loop, is
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$88.58/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$177.20 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.