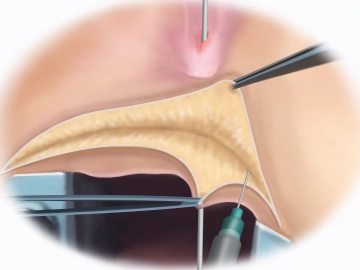
Start the procedure by inserting the rectal retractor and probing the rectovaginal fistula. In the video it connects the rectum with the lower third of the vaginal tube. Percutaneous injection of normal NaCl solution will facilitate the dissection. Follow this by opening up the perineum with a slightly curved incision with the needle-tip electrocautery. Transect the subcutaneous tissue and then install the Lone Star Retractor System™.
-
Probing the fistula, saline injection and transverse perineal incision
-
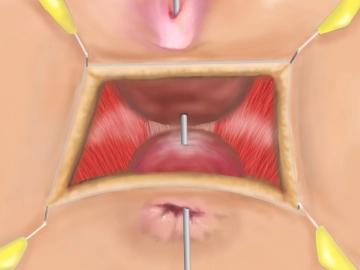
Dissecting the rectovaginal space and exposing the external sphincter and puborectalis
![Dissecting the rectovaginal space and exposing the external sphincter and puborectalis]()
Soundsettings Dissecting the rectovaginal space and exposing the external sphincter and puborectalis by carrying the dissection beyond the fistula tract, this allows reliable identification of the levator ani lateral to the vagina and anorectum. The goal is to have the levator limbs act as a barrier between the posterior wall of the vagina and the anterior wall of the rectum, as described in the following steps.
Before repairing the sphincter, locate the muscle stumps. Dissection is facilitated by injecting sa
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$88.58/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$177.20 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.