n rectal prolapse the rectum protrudes through the anus due to flaccid pelvic floor muscles and excessive straining. In rare cases the protruding rIectum may become incarcerated, necessitating emergency surgery. Prolonged prolapse may damage the sphincters to the extent that they can no longer retain stools (fecal incontinence).
Treatment initially entails avoidance of straining through management of bowel movement. But surgery is needed in most cases. Depending on patient age and severity of symptoms, abdominal and perineal/transanal surgical procedures may be employed.
-
Rectal prolapse
![Rectal prolapse]()
-
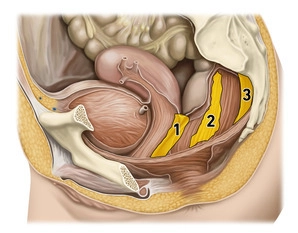
Pelvic floor
![Pelvic floor]()
(1) Rectoprostatic/rectovaginal fascia, (2) Paraproctium), (3) Mesorectal fascia
Acting as a "functional unit" the muscular pelvic floor closes off the inferior abdominal cavity and prevents the prolapse of intestines and pelvic organs. The structures of the pelvic floor support the intestinal and urogenital outlet system, with the muscular parts playing an essential functional role in retention and continence. Muscular overstretching and denervation may result in pelvic floor descent or the various forms of lesser pelvis organ prolapse. The incidence in women is far higher than in men (ration 9:1).
Pelvic floor dysfunction usually arises as a multifactorial process. The most common causes of pelvic floor disorders include multiparity, excessive straining during defecation, obesity, and prior pelvic surgery
-
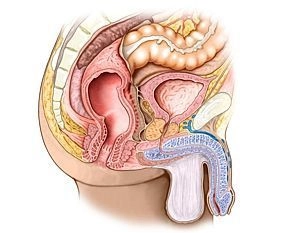
Rectum
![Rectum]()
Functionally, the rectum is a reservoir for feces preventing its continuous discharge. The rectum is continuous with the sigmoid colon and resembles it in that it has an S-shaped anteroposterior and lateral curvature (sacral, anorectal and sacral flexure). Typically, the rectum is subdivided into three segments:
1. Rectal ampulla (main reservoir, anterior to the sacrum)
2. Anal canal (see below; sealing zone between the anorectal flexure and the anal verge)
3. Between 1. and 2. an unspecified segment emerging at right angles from 1. and joining 2, also at right angles. Here, the mucosa presents with typical folds (Kohlrausch folds).
Posteriorly the rectum is related to the sacrum and coccyx, laterally to the internal iliac arteries and veins, regional lymph nodes, sacral plexus, and parts of the autonomic nervous system, as well as both ureters and uterine adnexae. In the female, the uterus and vagina lie anteriorly, while in men this is true for the bladder and prostate/seminal vesicles. Inferiorly the rectum is related to the pelvic floor.
(1) Tunica muscularis, longitudinal sublayer, (2) Tunica muscularis, circular sublayer, (3) levator
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$87.98/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$176.00 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.