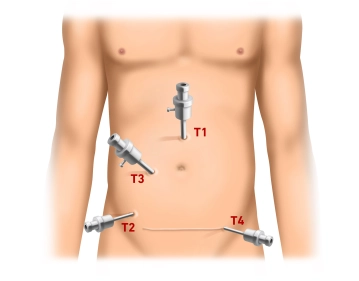
The procedure starts with a minilaparotomy for the camera trocar (T1, 10mm) about 3cm cephalad of the navel. After inserting the trocar, establish pressure-controlled pneumoperitoneum up to 13mm Hg and inspect the abdominal cavity for possible adhesions (e.g., after abdominal hysterectomy via Pfannenstiel incision). Successively introduce the working trocars under laparoscopic view: T2 (5mm) right lower quadrant at the level of the anterior superior iliac spine, T3 (10mm) roughly centered on a slightly curved line connecting T1 and T2. Finally insert T4 (5mm) in the left lower quadrant suprasymphyseally in the course of the subsequent Pfannenstiel incision.
-
Pneumoperitoneum and trocar positioning
-
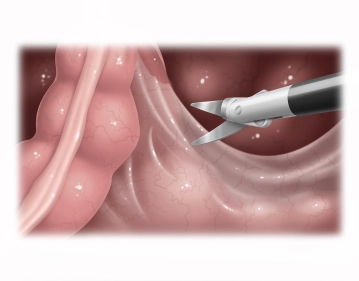
Opening the right pelvic peritoneum
![Opening the right pelvic peritoneum]()
Soundsettings Tilt the operating table to Trendelenburg, and with two atraumatic grasping forceps pull the greater omentum and small intestine into the upper quadrants or right middle abdomen. Pull the sigmoid colon (the video demonstrates a quite elongated sigmoid) to the left, thereby putting traction on the rectum and lifting it superiorly. With bipolar scissors (optionally: LigaSure® or BowaNightKnife®) open the right pararectal peritoneum at the promontory, identify the right ureter and iliac vessels, and carry the incision inferiorly along the peritoneal reflection. Open the posterior fascial space between the parietal pelvic fascia (Waldeyer fascia) and mesorectum as much as possible.
Note
- Identify the ureter before dissection is started, but it is not necessary to dissect it free or encircle it with a tape.
- The lateral support of the descending colon should be left intact to prevent later descent into the lesser pelvis.
-
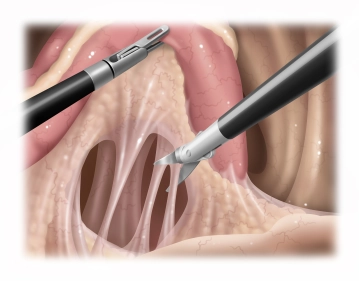
Mobilizing the posterior rectum
The incision of the anterior peritoneal reflection and subsequent dissection of the rectum in the a
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$87.56/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$175.10 / yearly payment