Viewed functionally, by acting as a reservoir for feces the rectum prevents continuous fecal expulsion. The rectum is continuous with the sigmoid colon and its S-shaped a/p and lateral curvature (sacral, anorectal and lateral flexure respectively) resembles that of the sigmoid. Usually, the rectum is divided into three sections:
1. Rectal ampulla (main reservoir, anterior to the sacrum)
2. Anal canal (see below, closure region between the anorectal flexure and cutaneous anal verge)
3. Between 1. and 2. an unnamed section emerging at right angles from 1. and transitioning into 2, also at right angles. Here, the mucous membrane displays characteristic folds (valves of Houston).
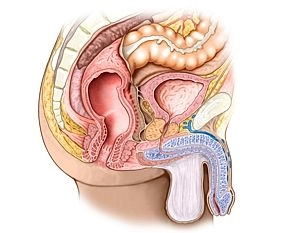
The gross relations of the rectum are: Posteriorly sacrum and coccyx, laterally the internal iliac artery and vein and the regional lymph nodes, the sacral plexus, and parts of the autonomic nervous system as well as the ureters and uterine appendages. In women the rectum is related anteriorly to the uterus and vagina, and in men to the bladder and prostate gland/seminal vesicles. It is delimited inferiorly by the pelvic floor.