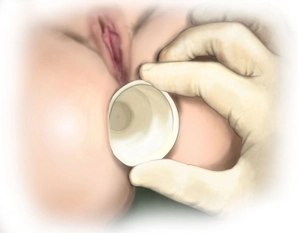
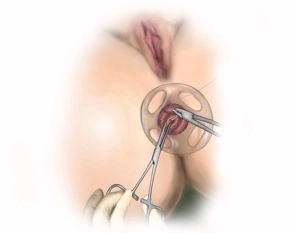
Perform a digital rectal examination to verify the findings and carefully dilate the anus digitally. During the digital rectal examination, the rectocele can be palpated anteriad, while the posterior wall of the vagina bulges into the rectum. The extent of rectoanal intussusception is assessed with dressing forceps and/or an Allis clamp. Now carefully dilate the anal sphincter with fingers before inserting the anal dilator. Introduce the transparent proctoscope into the anal canal as an anal port and for protection of the anoderm.
Note: The transparent proctoscope (anal port) may be temporarily anchored to the perianal skin with four stitches.