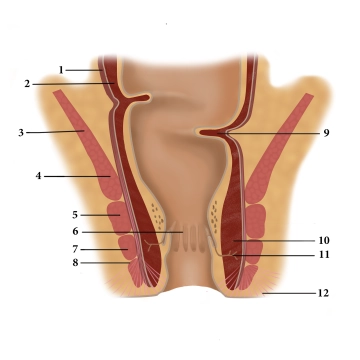
(1) Longitudinal muscular layer, (2) Circular muscular layer, (3) Levator ani muscle, (4) Puborectalis muscle, (5) Deep external anal sphincter, (6) Anal columns, (7) Superficial external anal sphincter, (8) Subcutaneous external anal sphincter, (9) Kohlrausch's fold, (10) Internal sphincter, (11) Proctodeal gland, (12) Corrugator ani muscle
Rectum
Functionally, the rectum serves as a fecal reservoir, preventing continuous defecation. It directly follows the sigmoid colon and, like it, has an S-shaped anterior/posterior and lateral curvature (sacral, anorectal, and lateral flexures). Typically, the rectum is divided into three sections:
- Ampulla recti (main reservoir, ventral to the sacrum)
- Anal canal (see below, closure region between the anorectal flexure and the skin opening)
- between 1 and 2, an unspecified section that emerges at a right angle from 1 and transitions at a right angle into 2. Here, typical folds (Kohlrausch's folds) are found in the mucosa.
Adjacent structures of the rectum include posteriorly the sacrum and coccyx, laterally the regional lymph nodes beside the internal iliac artery and vein, the sacral plexus, and parts of the autonomic nervous system, as well as the ureter and adnexa. Ventrally, in females, the uterus and vagina are located, and in males, the bladder and prostate/seminal vesicle. Caudally is the pelvic floor.
Read here more about the histology of the rectum.
Anal Canal
Three muscles form the closure apparatus in the wall of the lower rectum:
- The internal anal sphincter is a thickening of the last circular fibers of the smooth colon musculature and is innervated by the sympathetic nervous system.
- The levator ani muscle, on the other hand, is voluntarily innervated (sacral plexus), and the puborectalis muscle attached to the pubic bone is also included. It forms a large sling around the anal canal, bending it functionally forward.
- The external anal sphincter is also striated and suspended between the perineal center (perineal body) and the coccyx. It is voluntarily innervated by the pudendal nerve. Its contraction closes the anal canal terminally.
The different innervation of the three closing muscles provides additional security against failures and resulting incontinence.
Numerous longitudinal folds (anal columns) are found in the mucosa of the anal canal, which have dense arterial (!) plexuses with venous drainage. When the sphincter muscles contract, they quickly fill, and the mucosa swells, adheres, and thus provides a gas-tight closure. Hemorrhoids and venous thromboses are known vascular complications of this region.
Defecation occurs through the relaxation of the closure mechanisms (initiated by voluntary muscles, emptying of the erectile tissue) and through active abdominal press and intestinal peristalsis.
Vascular Supply
The rectum is supplied arterially by three main vessels:
- the superior rectal artery (from the inferior mesenteric artery) via the sigmoid mesocolon (note: transection of this artery at the level of the sigmoid leads to ischemia of the upper rectum!)
- the middle rectal artery (from the internal iliac artery), running cranially to the levator ani muscle
- the inferior rectal artery (from the internal pudendal artery), below the levator ani muscle
Under the mucosa of the rectum, the veins run as the rectal venous plexus. They drain the blood of the organ in the upper section as the superior rectal vein via the inferior mesenteric vein to the liver, in the middle and lower sections via the middle and inferior rectal veins and via the internal iliac vein to the inferior vena cava (portocaval anastomosis). Medications applied via suppositories thus only enter the organism unmetabolized if they are not pushed into the drainage area of the superior rectal vein.
Corresponding to the vascular supply, the lymph of the rectum is also drained: The large group of inferior mesenteric lymph nodes forms its own group (superior rectal lymph nodes) at the upper rectum, likewise, the internal iliac lymph nodes take lymph from the middle rectum (from the pararectal lymph nodes), and the superficial inguinal lymph nodes take lymph from the lower anal region, anus, and skin of the perineal region.
Perineal Region
The perineal region encompasses the area caudal to the pelvic diaphragm (urogenital and anal region) and is bounded
- cranially by the inferior pelvic diaphragm fascia
- ventrally by the symphysis
- laterally by the ischium
- dorsally by the lower edge of the gluteus maximus muscle
The posterior perineal region corresponds to the anal region and is termed the ischioanal fossa in nomenclature, while the anterior perineal region corresponds to the pubic region and can be further divided into three overlapping sections: the most superficial is a subcutaneous perineal space (between subcutaneous fascia = Colles' fascia and perineal fascia = Buck's fascia), a superficial perineal space between the perineal fascia and perineal membrane, and a deep perineal space cranial to the perineal membrane
The dorsally located ischioanal fossa consists mainly of adipose tissue and numerous vessels/nerves (branches of the inferior rectal artery and the internal pudendal artery as well as the pudendal nerve to the anal region). At the transition to the sacral region, an epithelial-lined cavity can form as a duct between the tip of the coccyx and the anal margin. This can be encapsulated as a cyst (pilonidal cyst/dermoid cyst) or can have an external connection (pilonidal fistula).
The ventrally located superficial perineal space (superficial perineal pouch) contains the superficial perineal muscles and the conduits to the external genital organs (perineal artery and artery of the bulb of the vestibule as well as branches of the pudendal nerve to the labia/clitoris or to the scrotum).
The ventral deep perineal space (deep perineal pouch) is less clearly defined, transitions dorsally into the ischioanal fossa, and contains the deep perineal muscles and further profound conduits.