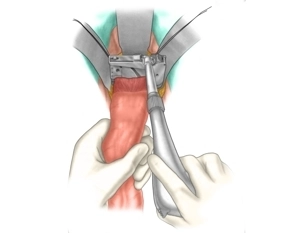
The technique is illustrated with descendorectostomy serving as an example (see also open rectal resection). The rectum is transected with a linear stapler.
-
Resecting the rectum
-
Dissecting the wall of the descending colon
Arming the proximal stump with a purse-string suture
First, clean and disinfect the proximal stump of the large bowel with a swab (e.g., soaked in povid
First, clean and disinfect the proximal stump of the large bowel with a swab (e.g., soaked in povid
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
US$9.40
inclusive VAT
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
from US$7.29 / module
US$87.56/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$14.59
/ month
US$175.10 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.