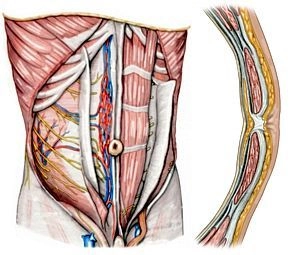
1. Muscles of the anterior abdominal wall
Rectus abdominis muscle: straight abdominal muscle invested by the rectus sheath with its three to four tendinous intersections (intersectiones tendineae) conjoined with the anterior lamina of the rectus sheath.
Pyramidalis muscle: originates at the superior pubic ramus, inserts in the linea alba, is situated anterior to the rectus abdominis and invested by its own sheath in the anterior lamina of the rectus sheath.
2. Layered anatomy of the anterior abdominal wall
Rectus sheath: Invests the rectus abdominis muscle; craniad to the midpoint between the umbilicus and pubic symphysis, the sheath divides into an anterior and posterior lamina. The posterior lamina ends there in the shape of the arcuate line; craniad to this line, the abdominal external oblique inserts in the anterior lamina of the rectus sheath, the abdominal internal oblique in both the anterior and posterior laminae, and the transverse abdominal muscle in the posterior lamina.
Semilunar (Spigelian) line: Transition zone between the aponeuroses of the lateral abdominal muscles and the lateral edge of the rectus sheath.
Linea alba: About 1 cm wide firm band of connective tissue between the right and left rectus sheaths, extending from the sternum to the pubic symphysis.
Transversalis fascia: Craniad to the arcuate line, it covers the posterior lamina of the rectus sheath, while caudad it is in intimate contact with the rectus abdominis.
3. Internal relief of the abdominal wall
Median umbilical fold: Median fold of peritoneum extending from the umbilicus to the urinary bladder; the fold invests the median umbilical ligament (strand of connective tissue = remnant of the urachus).
Medial umbilical fold: Paired folds of peritoneum; each side investing the medial umbilical ligament = obliterated remnant of the paired umbilical artery.
Lateral umbilical fold: Paired folds of peritoneum; on each side craniad to the inferior epigastric artery, with its two accompanying veins each.
4. Vessels and nerves
a) Arteries
Superior epigastric artery: Extension of the internal thoracic artery, anastomoses with the inferior epigastric artery at the level of the umbilicus.
Inferior epigastric artery: Arises from the external iliac artery and courses, just like its superior counterpart, within the rectus sheath on the posterior surface of the rectus abdominis.
Superficial epigastric artery: Arises from the femoral artery and, after passing over the inguinal ligament, radiates into the subcutaneous tissue of the anterior abdominal wall.
Posterior intercostal arteries VI-XI and subcostal artery: Arise from the thoracic aorta; their terminal segments course obliquely caudad between the abdominal internal oblique and transverse abdominal muscles, and coming from the lateral aspect they extend into the rectus sheath, where they join with the superior and inferior epigastric arteries.
b) Veins
Superior epigastric veins: Parallel the eponymous artery; anastomose with branches of the inferior epigastric vein and empty into the internal thoracic veins.
Inferior epigastric vein: Branches into veins accompanying the inferior epigastric artery and empties into the external iliac vein.
Superficial epigastric vein: Parallels the eponymous artery (see above)
c) Lymphatics
Superficial lymphatics Craniad to the umbilicus, they course to the axillary lymph nodes and caudad to the inguinal lymph nodes.
Deep lymphatics Usually parallel the blood vessels, pass into the parasternal, lumbar, and external iliac lymph nodes.
d) Nerves
Intercostal nerves VI – XII: As ventral rami of the thoracic nerves VI - XII; they course posterior to the rib cartilages into the abdominal wall between the internal abdominal oblique and transverse abdominal muscles; motor branches supply the anterior and lateral abdominal muscles, and sensory branches the abdominal skin.
Iliohypogastric nerve, ilioinguinal nerve, and genitofemoral nerve: Involved in motor and sensory innervation of the inferior abdominal region and genitals.