Open the abdomen through an epigastric midline incision, with left periumbilical extension caudad After inserting the abdominal retractor system, explore the abdominal cavity and assess the location and extent of the primary tumor as well as any lymph node involvement and organ metastases.
-
Access
-
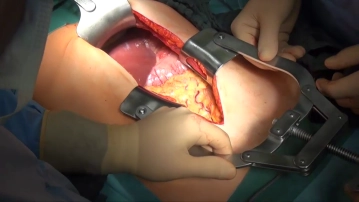
Freeing the greater omentum and transecting the gastroepiploic vessels
![Freeing the greater omentum and transecting the gastroepiploic vessels]()
Soundsettings Pull up the greater omentum and apply measured traction against the transverse colon. Dissect the greater omentum close to the upper aspect of the transverse colon and open the lesser sac.
After freeing the hepatic flexure and descending duodenum and carefully dividing the greater omentum off its adhesions with the mesocolon on the right, divide the gastroepiploic vessels entering here. Divide the right gastroepiploic vein before its union with the superior mesenteric vein, and the right gastroepiploic artery where it leaves the gastroduodenal artery. -
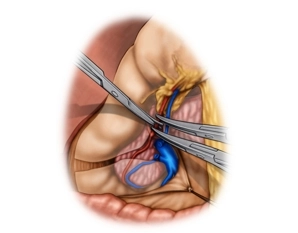
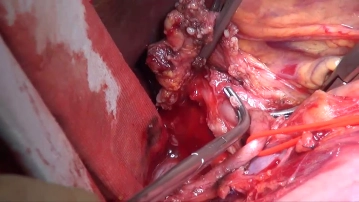
Lymphadenectomy I (hepatoduodenal ligament/LN stations 12 and 13)
![Lymphadenectomy I (hepatoduodenal ligament/LN stations 12 and 13)]()
Soundsettings Lymphadenectomy (LAD) starts at the hepatic hilum and continues along the hepatoduodenal ligament and common hepatic artery to the celiac trunk.
After the cholecystectomy, not demonstrated here, incise the lesser omentum with bipolar scissors close to the liver. Start the incision on the left side of the hepatoduodenal ligament and continue to the level of the cardia. With forceps lift the connective tissue together with all its lymph nodes (LN) anterior to the common hepatic artery at the left aspect of the hepatoduodenal ligament and expose the artery. Gradually dissect the LN tissue bundle (station 12) off the portal vein and common bile duct. After inserting the index finger into the omental foramen, palpate the common hepatic artery, hepatic artery proper, portal vein, and any possibly suspect lymph nodes with thumb and index finger. Now take down LN station 13 between the head of the pancreas and the portal vein.
-
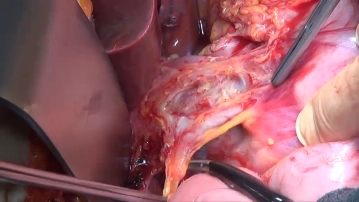
Lymphadenectomy II (common hepatic artery/station 8)
![Lymphadenectomy II (common hepatic artery/station 8)]()
Soundsettings Transect and ligate the right gastric artery between Overholt dissecting forceps. After encircling the hepatic artery proper with a vessel loop, pull the LN tissue bundle (station 8) craniomediad and with bipolar scissors gradually take it down completely along the common hepatic artery toward the celiac trunk. Since the lymph nodes are immediately adjacent to the adventitia, ensure that the dissection is carried out close to the latter. Encircling the common hepatic artery with a vessel loop simplifies the dissection. The posterior margin of the lymph node dissection is defined by the anterior aspect of the inferior vena cava.
-
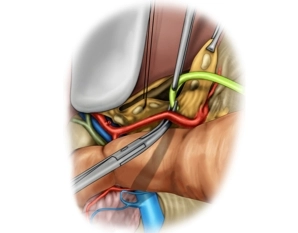
Lymphadenectomy III (celiac trunk/station 9)
![Lymphadenectomy III (celiac trunk/station 9)]()
Soundsettings Expose the common hepatic artery and splenic artery branching off the celiac trunk as described above and free them from the LN tissue bundle. Complete the LAD by taking down the left gastric artery close to its origin and delivering the LN tissue bundle. Do not fully expose the origin of the celiac trunk and the aorta.
After grasping the stomach with organ holding forceps on the large curvature, judiciously pull the
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$87.56/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$175.10 / yearly payment
TachoSil® is used in adults and children from 1 month of age as supportive treatment in surgery for
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$87.56/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$175.10 / yearly payment