- Primary gastric cancer
- Remnant gastric cancer
- Individual in resectable metastases, local peritoneal carcinomatosis (P1), recurrent malignancies (gastric stump cancer)
- Unless there are massive risk factors (previous disease or general condition of the patient, see contraindications), surgery is generally indicated if curative treatment and local resectability are feasible.
- Pre-/perioperative chemotherapy is recommended in locally advanced tumors.
- Palliative gastrectomy may be indicated in rare cases of palliation (e.g., bleeding, perforation, stenosis).
In order to achieve tumor-free resection margins (R0), a proximal safety distance in situ at the stomach of 5 cm (Lauren intestinal type) or 8 cm (Lauren diffuse type) must generally be maintained, except in mucosal carcinomas (T1a N0 M0). Lymph node clearance of compartments I and II is called D2-LAD and is the standard lymphadenectomy in gastric cancer. It can be regarded as the gold standard.
The extent of the resection (total versus subtotal gastrectomy) is determined by tumor location/spread and the safety margin required by the histologic type.
Special case of early gastric cancer
Early gastric cancer is defined as a tumor restricted to the mucosa and submucosa of the gastric wall irrespective of lymph node status, spread and distant metastasis. By definition the gastric tunica muscularis is tumor-free.
Early cancer differs with respect to the rate of potential lymph node metastasis. Tumors already infiltrating the submucosa are not candidates for endoscopic treatment, since there is a 4%–20% probability of lymph node metastasis.
About 5% of patients present with early gastric cancer of the mucosal type (pT1m), where a curative approach by endoscopic resection is possible as the probability of lymph node metastasis is extremely low. These patients have an excellent prognosis with a five-year survival rate of > 90%.
Indication for endoscopic resection
Superficial gastric cancer limited to the mucosa (about 5% of patients) and meeting the following criteria can be treated by endoscopic resection:
- Lesions < 2 cm in size in elevated tumors
- Lesions < 1 cm in size in flat tumors
- Histologic grade: Well or moderately differentiated (G1/G2)
- No macroscopic ulceration
- Invasion limited to mucosa
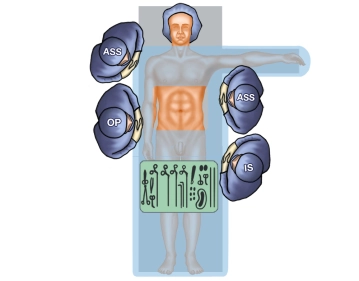
The case presented here was diagnosed with a 5 cm large ulcerated gastric tumor at the large curvature in the transition zone from the middle to the distal third of the stomach. Histology demonstrated gastric cancer of the Lauren intestinal type, with endosonographic tumor staging yielding uT2, with no evidence of lymph node/distant metastasis. Therefore, indication for gastrectomy with D2 lymphadenectomy.