Functionally, the rectum serves as a fecal reservoir, preventing continuous defecation. It directly follows the sigmoid colon and, like the latter, exhibits an S-shaped anterior-posterior and lateral curvature (sacral, anorectal, and lateral flexures). Typically, the rectum is divided into three sections:
1. Ampulla recti (main reservoir, ventral to the sacrum)
2. Anal canal (see below, closure region between the anorectal flexure and the skin opening)
3. Between 1 and 2, an unspecified section that emerges at a right angle from 1 and transitions at a right angle into 2. Here, typical folds (Kohlrausch folds) are found in the mucosa.
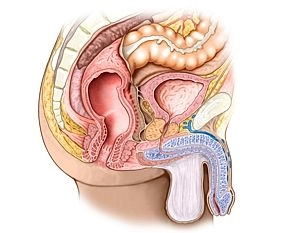
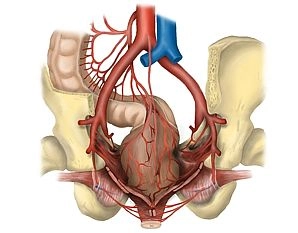
Adjacent structures of the rectum include dorsally the sacrum and coccyx, laterally the regional lymph nodes next to the internal iliac artery and vein, the sacral plexus, and parts of the autonomic nervous system, as well as the ureter and adnexa. Ventrally, in females, are the uterus and vagina, and in males, the bladder and prostate/seminal vesicle. Caudally is the pelvic floor.