NLR-Monitoring
For intraoperative neuromonitoring (IONM) of the recurrent laryngeal nerve (RLN), the vagus nerve or the RLN is electrically stimulated. The muscle action potentials triggered by the stimulation are derived as an electromyogram (EMG) from the intrinsic laryngeal muscles in the area of the vocal cords (M. vocalis) and transformed into an acoustic tapping signal. This can be done either by a needle electrode inserted into the M. vocalis through the cricothyroid ligament or by surface electrodes applied to the endotracheal tube. The IONM systems available on the market today also offer the possibility of visually displaying the EMG signal as a voltage-time curve on a monitor.
While in thyroid and parathyroid resections near the nerve, especially in total lobectomy, visual nerve representation still provides the best possible condition for sparing the RLN ("gold standard"), the IONM enhances the safety of the operation through two additional anatomical-functional applications:
- secure nerve identification
- assessment of nerve function and postoperative vocal cord function
For the IONM results to be indicative of postoperative vocal cord function, the following conditions must be met:
- correct functioning of the recording system regarding nerve stimulation and signal acquisition/playback
- exclusion of pre-existing or intubation-related non-neural impairments of vocal cord mobility
- strict standardization of the IONM
- appropriate cause analysis in case of disturbances
Standardization of Electrophysiological Recurrent Monitoring
The basic prerequisites for standardizing RLN monitoring include:
1. Pre- and postoperative laryngeal findings
Pre- and postoperative laryngoscopy and IONM form an inseparable diagnostic unit. The pre-resection intraoperative EMG finding is not interpretable without the preoperative laryngoscopy finding, nor is the post-resection EMG finding without the postoperative laryngoscopy finding.
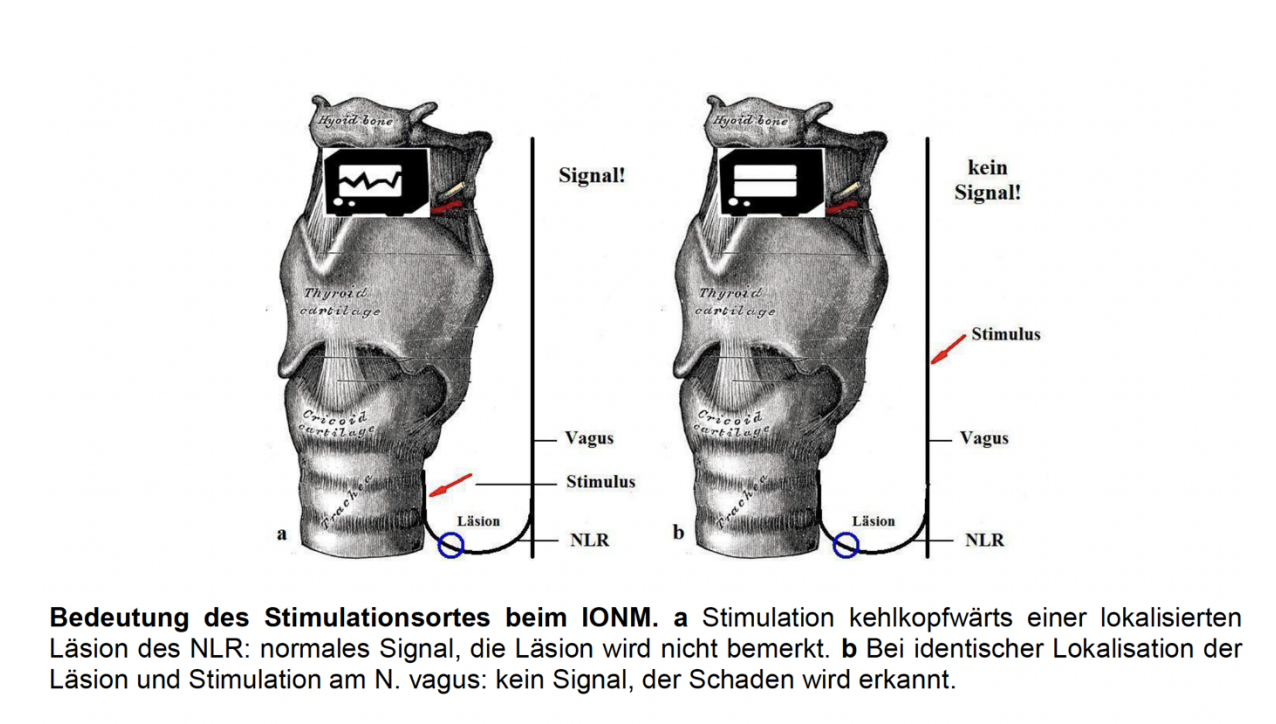
2. RLN stimulation must occur proximal to the potential damage area of the nerve, with ipsilateral stimulation of the vagus nerve being the safest.
3. Sufficient nerve stimulation requires a threshold current strength of at least 0.3-0.8 mA. Optimal current strengths range between 1 and 2 mA; further improvement of the muscle response of the M. vocalis is not achieved with higher current strengths.
4. During the neuromonitoring phase, muscle relaxants must be avoided as they impair the muscle response of the M. vocalis, leading to misinterpretations. Only short-acting relaxants should be used during intubation.
5. The recording system must function flawlessly. This includes the proper establishment of cable connections and the correct placement of neutral and signal recording electrodes:
- Needle electrodes: These must be inserted transligamentally into the M. vocalis separately for each operated side.
- Tubus electrodes: After positioning the intubated patient (head reclination), it must be ensured that the tube cuff is below the glottis level and the signal recording electrodes are above it, i.e., at the glottis level of the vocal cords.
6. Technically, EMG recording is a prerequisite for controlling proper nerve conduction and corresponding muscle action of the M. vocalis. The sole playback of the signal tone cannot reliably distinguish between proper muscle action potential and artifact signal.
From a surgical perspective, the following standard steps must be observed to make a prognostic statement about the expected postoperative vocal cord function:
- preoperative laryngoscopy finding
- ipsilateral stimulation of the vagus nerve with 1 - 2 mA with EMG recording
- Before starting the resection, visual representation and repeated ipsilateral stimulation of the RLN, possibly also of the ipsilateral vagus nerve.
- Stimulation of the vagus nerve and EMG recording after completion of all ipsilateral surgical measures
- postoperative laryngoscopy finding
Cause Analysis in Intraoperative Signal Loss
If there is an intraoperative signal loss with initially proper signal response, it must be investigated. A standardized approach is also recommended here:
1. Exclusion of anesthesia-related neuromuscular blockade, technical device malfunction, dislocation of cable connections or neutral electrode, dislocation of the tube with tube electrodes, or dislocation of the needle electrodes
2. Stimulation of the RLN just before its entry point into the larynx and away from the entry point, as well as stimulation of the ipsilateral vagus nerve; additionally, palpation of the dorsal laryngeal wall to verify a stimulation response (muscle twitch = laryngeal twitch, considered a positive sign of muscle action of the M. vocalis). Depending on the stimulation site and response, the following conclusions can be drawn:
- Muscle twitch of the posterior laryngeal wall indicates a recording error of the stimulation response, for example, tube dislocation with tube electrodes, needle dislocation with needle electrodes.
- Positive muscle twitch and/or proper EMG at RLN stimulation at the entry point into the larynx, but missing stimulation response at the entry point distant RLN stimulation or over the vagus nerve indicates with high probability a true functional loss of the ipsilateral RLN; through "mapping," the site of nerve disturbance can usually be pinpointed.
- Lack of muscle twitch and lack of EMG response regardless of the stimulation site (RLN or vagus nerve) means, after excluding the causes mentioned under 1), a diffuse nerve disorder or at least a transient postoperative recurrent paresis.
In the signal loss forms explained under b) and c), a transient recurrent paresis results in 40 - 70% and a permanent recurrent paresis in 10 - 20%.
- If there is uncertainty regarding the device technology or the position of the needle electrodes or the tube, stimulation of the contralateral vagus nerve can provide clarity: If the stimulation of the contralateral vagus nerve/RLN was initially and also during this control unremarkable, a device error is excluded, and a disturbed nerve function of the opposite side must be assumed.
Conclusion: If the IONM was performed correctly and resulted in a flawless signal response at the end of the operation, postoperative recurrent paresis is extremely rare. In case of intraoperative signal loss not attributable to a device or user error, transient recurrent paresis must be expected in 1/3 of cases and permanent recurrent paresis in 1/10 of cases.
The AWMF guideline "Surgical Treatment of Benign Thyroid Diseases" as of 12/2021 requires:
"The gentle, i.e., non-skeletonizing, nerve blood flow-preserving preparative representation of the RLN reduces the risk of damage and should generally be performed in both primary and recurrent interventions. The visualized anatomical nerve course should be documented before and after resection. Exceptionally, representation can be omitted if the resection plane is at a safe distance ventral to the lateral boundary lamella to the nerve course. The non-representation of the RLN should be documented with justification."
Intraoperative neuromonitoring (IONM) does not replace the gold standard of visual nerve representation but is used in addition to it. The procedure can reliably confirm the identity of the RLN and make its functionality very likely with an undisturbed conduction signal, whereby stimulation over the vagus nerve after resection is required to capture the entire nerve course. For legal reasons, it is recommended to store the derivation of electromyograms in paper or electronic form. The use of IONM allows for a planned bilateral operation and signal loss on the first side to review the strategy (e.g., staged surgical approach, which can reduce the risk of bilateral recurrent paresis).
EBSLN-Monitoring
Intraoperative neuromonitoring (IONM) of the external branch of the superior laryngeal nerve (EBSLN) serves to identify and test the function of the nerve to avoid damage during thyroid or parathyroid surgery.
The EBSLN innervates the cricothyroid muscle. It is crucial for the tension of the vocal cords by tilting the thyroid cartilage forward.
Damage does not lead to classic hoarseness as with the RLN but to a reduced ability to modulate the voice and reach high frequencies.
The loss of high pitches is particularly problematic for voice professionals such as singers or speakers.
Methods of derivation: After electrical stimulation of the nerve, EMG signals are derived from the M. cricothyroideus.
A) Direct derivation via needle electrode
- Intramuscular electrode in the M. cricothyroideus, resulting in high sensitivity but requiring additional access to the muscle.
B) Surface derivation via EMG tube
- less specific for the EBSLN
- Can be combined with nerve monitoring of the RLN
Course of operation with monitoring:
Step 1: Identification of the EBSLN
- The EBSLN runs parallel to the superior thyroid artery and extends to the M. cricothyroideus.
- Stimulation occurs before ligation of the upper polar artery, as the nerve is particularly at risk here.
- Variable course of the nerve (Cernea classification):
The Cernea classification describes the anatomical location and risk of injury of the external branch of the superior laryngeal nerve (EBSLN) in relation to the upper polar artery of the thyroid.- Type 1: High course → lower risk of injury.
- Type 2a/2b: Close to the upper polar artery → higher risk.
Step 2: Stimulation with the probe
- Stimulation with 1 – 2 mA
- An intact nerve leads to contraction of the M. cricothyroideus, which can be noticed by:
- Palpation of the muscle (in open surgery)
- Measurement of an EMG signal via derivation electrodes
Step 3: Interpretation of the signals
- Positive signal → The nerve is functionally intact, no further risk.
- Weak or absent signal → Indication of possible damage or anatomical variant.
Step 4: Post-resection check
- After ligation of the upper polar artery, a renewed stimulation is performed.
- Persistent signals = function-preserving operation.
- Signal loss = potential nerve damage → postoperative voice training may be required.
Conclusion: EBSLN monitoring should be used especially in thyroid surgeries with difficult anatomy and in patients with high vocal demands. It helps to avoid postoperative voice problems and increases safety in surgery.