The human pelvis is a complex ring structure that fulfills two main functions. On one hand, it forms the lower closure of the trunk and thus carries the weight of the upper body. On the other hand, it transfers this weight to the lower limbs, which is crucial for the upright posture and locomotion of humans.
The pelvis is composed of several bony elements. The foundation is formed by the two hip bones, also known as the pelvic girdle or cingulum membri inferioris. Between them is the sacrum. The os coxae consists of three main components:
1. The ilium (Os ilium), consisting of the corpus ossis ilii and the ala ossis ilii.
2. The ischium (Os ischii), consisting of the corpus ossis ischii and the ramus ossis ischii.
3. The pubis (Os pubis), consisting of the corpus ossis pubis, the ramus superior, and the ramus inferior ossis pubis.
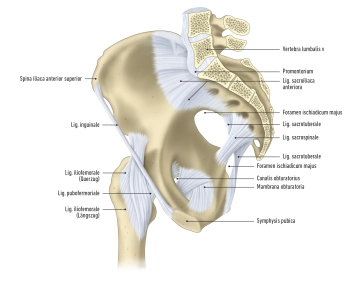
These bones and the sacrum are connected by various types of connections, including ligamentous connections, cartilaginous connections, and joints:
1. Ligamentous connections include the membrana obturatoria, the ligamenta sacroiliaca, sacrotuberale, and sacrospinale.
2. Fibrocartilaginous connections are established by the symphysis pubica.
3. Joint connections include the articulation sacroiliaca and the articulatio sacrococcygea.
There are various ligaments involved in the joints:
- The ligg. sacroiliaca anteriora and posteriora are ligaments that connect the upper and lower ends of the ilium to the sacrum.
- The ligg. sacroiliaca interossea extend between the sacrum and the tuberositas ossis sacri and tuberositas iliaca.
- The lig. iliolumbale runs from the 4th and 5th lumbar vertebrae to the crista iliaca and the tuberositas iliaca.
- The ligg. sacrotuberale et sacrospinale are additional ligaments that act on the articulatio sacroiliaca.
- The lig. sacrococcygeum anterius, the lig. sacrococcygeum posterius profundum, and the lig. sacrococcygeum posterius superficiale are ligaments that connect the sacrum to the coccyx.
The pelvis is divided into two main parts:
- the greater pelvis (pelvis major) and
- the lesser pelvis (pelvis minor).
The linea terminalis is the dividing line between them. The greater pelvis, above the linea terminalis, contains the space between the two iliac wings, while the lesser pelvis includes the pelvic inlet, the pelvic outlet, and the pelvic walls.
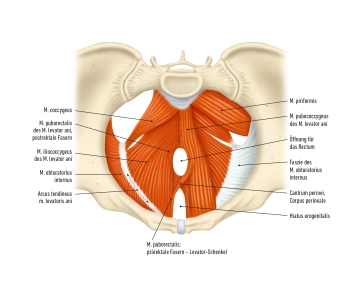
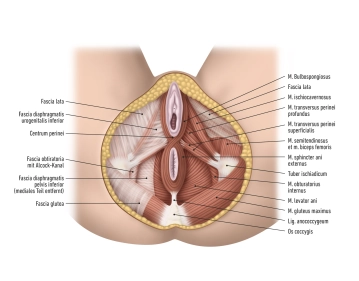
The pelvic walls are covered by connective tissue, known as fasciae. These fasciae are important for the stability and delineation of the pelvic organs. Furthermore, there are openings in the pelvic walls that allow the passage of blood vessels, nerves, and muscles that run between the pelvis and the buttocks. The pelvic region is rich in neurovascular structures that play an important role in supplying the pelvis and lower extremities.