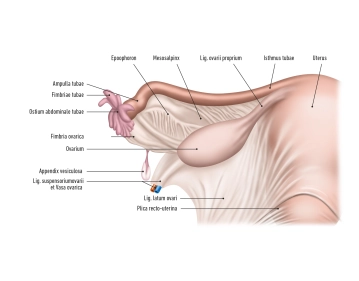
The ovary (Ovarium) is located laterally in the pelvic region and runs in a vertical orientation. It has an inner surface facing the interior of the pelvis (Facies medialis/intestinalis) and an outer surface directed towards the lateral pelvic wall (Facies lateralis). The rounded free edge is referred to as the Margo liber, and at the anterior edge, the Margo mesovaricus, the mesovarium is attached, which is a structure of the broad ligament of the uterus (Lig. latum uteri).
There are two poles:
- Extremitas uterina
- Extremitas tubaria
The hilum of the ovary, where vessels and nerves enter, is located at the attachment of the connective tissue of the ovary, known as the mesovarium, at the Margo mesovaricus.
The ovary is connected to the pelvic wall at the Extremitas tubaria by the suspensory ligament of the ovary. The ovarian vessels (Vasa ovarica), lymphatic vessels, and nerves run along this suspensory ligament.
The proper ovarian ligament lies between the ovary (Extremitas uterina). This is located directly behind the tubal angle. The artery R. ovaricus of the uterine artery runs here.
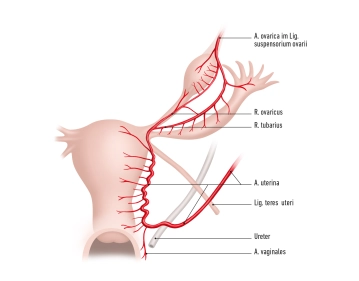
The ovary is supplied by:
- A. ovarica
- Ramus ovaricus from the uterine artery.
These arteries form anastomoses at the Margo mesovaricus and supply the ovary with blood.
Veins transport the venous blood via the right ovarian vein to the inferior vena cava and via the left ovarian vein to the left renal vein. Part of the blood flows through the uterine plexus to the internal iliac vein.
The ovary is located in the abdominal cavity (intraperitoneal) in the ovarian fossa. Here, in the retroperitoneum, run the obturator nerve, obturator vessels, and external iliac vessels. Medially, the umbilical artery and the uterine artery also run.