The uterus, also known as the womb, is a hollow, muscular organ in the female body that plays an important role during pregnancy and childbirth.
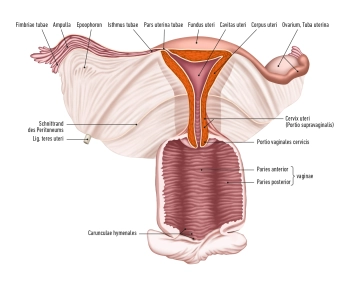
The uterus consists of:
- the body (Corpus uteri),
- the isthmus uteri
- the cervix (Cervix uteri)
The average length of the uterus is about 7.5 cm, the width 4 cm, and the thickness 2.5 cm.
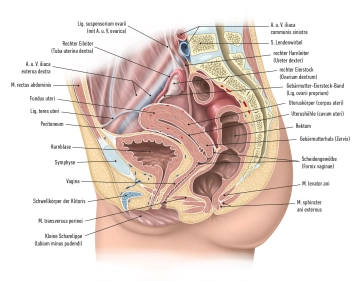
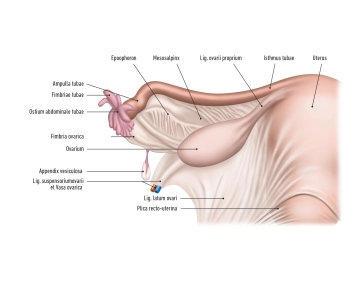
The fundus: uteri represents the upper section of the uterus, located above the entry points of the fallopian tubes. Its lateral walls are connected with the broad ligament (Ligamentum latum uteri). At the lateral edges of the uterus, where the fallopian tubes enter the uterus, the tubal angle is formed. From the tubal angle, the ligamentum ovarii proprium extends to the ovary, while the ligamentum teres uteri extends to the inguinal canal.
Cervix uteri: The cervix extends with its conical lower third into the vagina. It is divided into the portio supravaginalis cervicis (endocervix) and the portio vaginalis cervicis (ectocervix or simply portio). In the upper area of the vagina, the cervix uteri forms the anterior and posterior vaginal fornices (fornix vaginae) between the portio and the vaginal wall.
Portio vaginalis: At the end of the portio vaginalis is the external os, also known as the ostium uteri (orificium externum uteri).
The portio vaginalis normally has a reddish color and is covered with stratified non-keratinized squamous epithelium, similar to the vagina. At the transition to the ostium uteri, this epithelium changes to the single-layered columnar epithelium of the cervical canal (canalis cervicis). Between puberty and menopause, the cylindrical epithelium of the cervical canal can migrate outward onto the portio (ectropion), leading to a more intense redness. Precancerous lesions and cancer can be detected in this area with a colposcopy.