Principles and Technique of Flexor Tendon Repair
Adhesions and scarring between the tendon and surrounding tissue, especially in the area of the flexor tendon sheaths, are the main problem in flexor tendon surgery. Adhesions can only be avoided by early mobilization of the tendon through passive, preferably active, rehabilitation concepts [1]. Since the suture site is mechanically stressed even before the tendon has healed, high demands are placed on the stability of the suture.
If there is a rupture of the suture site, this is due to mechanical overload of the suture material in 80% of cases. Knot formations can reduce strength by up to 50% and lead to a significant weakening of the suture material [2]. In 20% of cases, the rupture of the suture site is due to a tear-out of the suture from the tendon tissue.
During functional rehabilitation, a gradual dehiscence may develop, i.e., a separation of the tendon stumps without rupture of the suture site. Dehiscences are caused by the loosening of the suture in the tendon and intratendinous scar formation. Scars within the tendon represent a weak point that can lead to a later functionally disturbing overlength of the tendons. If the dehiscence is more than 3 mm, the strength of the suture does not increase after the 10th postoperative day, leading to a high risk of rupture [3].
Factors that can significantly impair the gliding ability of the suture include:
- swelling of the suture site caused by overly tight core suture
- introduction of excessive amounts of suture material
- suture material and knots not embedded in the tendon tissue
- protruding fibers from the tendon stumps in the suture area
- dehiscences (see above)
The gliding ability of the tendon after reconstruction depends on the following parameters:
- technique of the core suture
- number of suture strands
- suture thickness, suture material
- technique of fine adaptation
For the technique of the core suture, it is true that thread guides, in which the thread encompasses the tendon fibers so that the loop closes when the suture is tightened (so-called locking suture), are significantly more stable than encircling sutures (10 – 50% [4, 5]). A classic example is the Kirchmayr-Kessler suture [6, 7]. The loop diameter should be greater than 2 mm, otherwise the loop may tear out [8]. Locking intermediate sutures can further increase suture strength but lead to uneven tension distribution in the suture, which can lead to overloading of tendon strands [9].
The strength of a suture increases with the strength of the suture material. Measurements on braided polyester threads show that the strength of a 4/0 suture is 64% higher than that of a 5/0 suture. A 3/0 thread has 43% higher tear strength than a 4/0 thread, a 2/0 thread compared to 3/0 by 63% [10]. Threads of 5/0 strength are not suitable for core sutures due to their low strength [11].
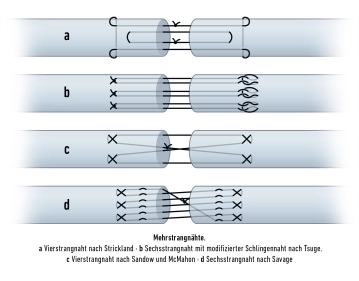
With the number of loops and knot formations within the tendon, the strength of a flexor tendon suture increases [12]. These interactions between thread and tendon are referred to as anchor points. Suture techniques with a significantly higher number of anchor points compared to the simple Kirchmayr-Kessler suture increase the stability of tendon reconstruction [13].
Various biomechanical studies have shown that the tear resistance of a flexor tendon suture increases proportionally with the number of suture strands, but decreases between the 5th and 21st day, independent of the number of suture strands, although at different levels depending on the suture technique [2, 14]. For postoperative care after flexor tendon suture, this means:
- The tear resistance of a two-strand suture is sufficient for the stresses of passive rehabilitation, but not for active rehabilitation without resistance.
- Only from a four-strand suture is there sufficient tear resistance for active rehabilitation without resistance.
- No suture technique offers sufficient stability for maximum force application.
For the position of the knots, they should be embedded in the tendon. Regarding tendon gliding ability, it is most favorable if the knots are located in the suture site itself. However, this causes some dehiscence, and a knot reduces the contact area of the tendon stumps. If two knots are placed in the suture site, the contact area is reduced by up to 27%, with the eight-strand suture according to Savage by up to 18%, with the Kirchmayr-Kessler suture by 2% [15, 16]. However, it is generally not a problem to embed the knot outside the suture site as in the modification of the Kirchmayr-Kessler suture according to Zechner, demonstrated in the OP procedure, step 6 in the clip [17].
The durability of the tendon suture also depends on the knot technique. A surgical knot tied 4 times is recommended [12]. A knot tied 4 times per suture provides higher tear resistance than multiple knots per suture, which is attributed to uneven distribution of suture tension and a decrease in tear resistance in the knot itself [2, 18, 19]. Placing the sutures in the dorsal portions of the tendon is said to lead to higher stability [20, 21].
After a tendon transection, degenerative changes occur in the adjacent sections of the tendon stumps, leading to a decrease in strength, which is why the anchor points should not be placed too close to the tendon stump. The most favorable position of the anchor points is at a distance of 7 to 10 mm from the tendon stump. A greater distance (> 12 mm) does not result in greater strength [22, 23].
After performing the core suture, a circumferential fine adaptation should be performed to smooth the surface, increase tear resistance, and prevent dehiscences, in which the superficial tendon portions are inverted [24, 25, 26]. Fine adaptation must be performed with the finest suture material to not impair the gliding ability of the tendon by the external suture material.
There is currently no consensus on the optimal suture material for flexor tendon surgery. Commonly used non-absorbable suture materials include braided polyester threads, monofilament nylon, monofilament polypropylene, and threads made of braided polyethylene. For absorbable threads, sufficient material endurance must be considered, which is achieved, among others, by polydioxanone and polylactide [27, 28, 29].
Principles for Performing Flexor Tendon Sutures
more favorable | less favorable | |
Thread course in the tendon | locking sutures, locking intermediate knots | encircling sutures |
Strength of the suture material | thread strength 3/0 and 4/0 | thread strength 5/0 and 2/0 |
Anchor points | large number, e.g., cross-stitch suture according to Becker | small number, e.g., Kirchmayr-Kessler suture |
Number of suture strands | ≥ 4 | 2 |
Knot position | in the tendon | outside the tendon |
Distance of anchor point from tendon stump | 7-10 mm | < 7 mm |
circumferential fine adaptation suture | yes | none |