The long flexor muscles of the fingers originate at the ulnar epicondyle of the humerus. Two tendons attach to each finger. The superficial flexor tendon splits into two slips and ends at the base of the middle phalanx, the deep flexor tendon passes through the split superficial one and attaches to the palmar base of the distal phalanx.
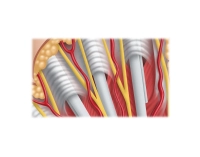
The flexor tendons are enveloped by tendon sheaths in the palm and on the fingers. They enable low-friction gliding with high amplitude and ensure a constant bone-close position of the flexor tendons, even during finger movement. Reinforcing annular ligaments are integrated into the tendon sheaths.
Radial and ulnar to the flexor tendon sheath runs the digital vessel/nerve bundle. At the level of the distal palm, the nerves lie palmar in the transverse plane, the arteries dorsal. They are located 2 to 5 mm lateral to the flexor tendon sheath and are therefore at risk of injury during surgical procedures.
The pulley system consists of a synovial-lined sheath around the flexor tendons, extending approximately from the metacarpal neck to the distal interphalangeal joint. The sheath is stiffened by fibrous reinforcements (stratum fibrosum), which are found at various intervals along the entire length.
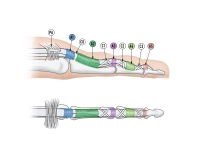
These structures are either transverse or oblique in orientation. Usually, the transverse reinforcements are referred to as "annular ligaments" (Lig. anulare) and the obliquely running ones as "cruciate ligaments" (Lig. cruciforme), regardless of whether the oblique reinforcements are truly cruciform (x-shaped) or consist only of oblique fibers in a single orientation.
Numerous anatomical studies have confirmed that at the palmar plate of the individual finger joints there is always an annular ligament present. Annular band structures are also regularly found on the shafts of the proximal and middle phalanges. These are designated from proximal to distal position as A-1, A-2, A-3, A-4, and A-5. The cruciate ligaments are also numbered, from proximal to distal as C-1, C-2, and C-3. C-1 and C-3 lie distal to the A-2 or A-4 band and are attached proximally to the phalanx and distally to the palmar plate. The cruciate ligaments located proximal to the A-2 and A-4 annular ligaments are less regularly found. A distinct gap between the A-1 and A-2 annular ligament is found in 40 to 90% depending on the cited study and is sometimes referred to in the literature as C-0. The C-3 cruciate ligament occurs more regularly than C-0, but varies in its form.
The A-2 annular ligament is the longest band and accounts for about 40% of the length of the proximal phalanx.
The A-1 annular ligament measures on average about 6 mm (4-8 mm) and thus corresponds to about 20% of the proximal phalanx length.
The function of the annular ligaments is to guide the flexor tendons closely to the bony skeleton, thereby ensuring optimal force transmission and mobility of the fingers. In this, the A-2 annular ligament, as the longest, plays the most important biomechanical role. The cruciate ligaments prevent collapse and allow expansion of the tendon sheath during digital movements. They facilitate the approximation of the annular ligaments during maximum flexion.
This finely tuned movement system is massively disrupted in stenosing tenosynovitis, the so-called trigger finger. A nodule formation of the flexor tendons directly proximal to the tendon sheath entrance leads to mechanical irritation of the A1 annular ligament with consecutive stenosis. The gliding ability of the flexor tendons is impaired, resulting in a snapping phenomenon.
The primary therapeutic approach is conservative and includes local infiltration of cortisone in the area of the A-1 annular ligament. This leads to good results especially at the beginning of the disease, the tendon nodule becomes smaller and the tendon runs smoothly again in the tendon canal. However, if a mechanical narrowing has already developed, the cortisone therapy is only of short duration. A surgical opening of the narrowing, the A-1 annular ligament division, is necessary to eliminate the entrapment.