- Intestinal angina due to short segmental stenosis of the superior mesenteric artery (SMA) close to its origin or occlusion due to inadequate collateral blood supply via the celiac trunk
- Lack of indication for interventional treatment, e.g., in long stenosis at the origin stenosis/occlusion of the SMA).
- Failure of interventional management
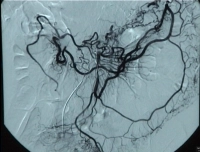
Video clip: SMA occlusion close to its origin with occlusion of the celiac trunk
Grade of ischemia and general indication for surgery
| Stage | Symptoms | Indication for surgery |
| I | Asymptomatic | Optional in concurrent procedures for vascular occlusion, aortic or iliac artery interventions |
| II | Intestinal angina = crampy postprandial abdominal pain, cachexia | Absolute indication for surgery |
| III | Abdominal pain at rest | Absolute indication for surgery |
| IV | Acute abdomen secondary to mesenteric infarction, intestinal gangrene, possibly peritonitis due to transmural bacterial translocation | Emergent indication for surgery |