General surgical risks
- Major bleeding, blood transfusions, transmission of hepatitis/HIV through allogeneic blood transfusions
- Allergy/intolerance
- Wound infection
- Thrombosis/embolism
- Skin/vascular/nerve damage, e.g., due to patient positioning
- Keloids (in open surgery)
Specific procedural risks
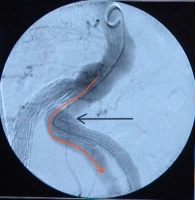
- Vascular injuries, e.g., during graft delivery: surgical hemostasis, blood transfusions, in case of massive bleeding or arterial rupture, immediate conversion to open surgery
- Pseudoaneurysm of the punctured vessels, arteriovenous fistula, seroma
- Inadequate graft fixation or leakage: corrective procedures, possibly open surgery
- Graft infection: possible after days, months, or even years; endocarditis, sepsis, leg ischemia, amputation; surgical removal of vascular graft
- Nerve lesions -> dysesthesia; pain; paralysis of abdominal wall / thigh muscles
- Lymph fistula
- Temporary or permanent lymphedema of the legs; compression stockings, lymphatic drainage
- Secondary bleeding
- Impotence
- Deterioration of renal function induced by intraoperative angiography, chronic dialysis
Risks due to impaired perfusion
- Thrombosis/embolism: pulmonary embolism, apoplexy, myocardial infarction; prophylaxis: heparin → HIT II risk
- Legs: thrombosis of the graft and possibly adjacent vascular segments, possibly leg ischemia, amputation (e.g., toes)
- Gluteal muscles: due to overstenting of the iliac arteries, in particular bilaterally; claudication during walking, possibly gluteal necrosis