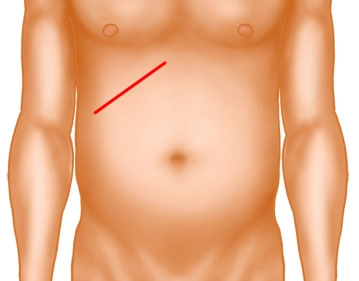
The preferred access is an upper transverse incision. Whenever needed the incision may be extended to the left as far as necessary. Before laparoscopic cholecystectomy became the gold standard, the recommended access was the right oblique subcostal (Kocher) incision (se figure above).
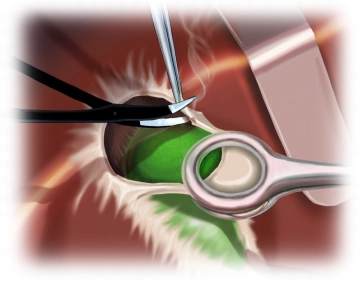
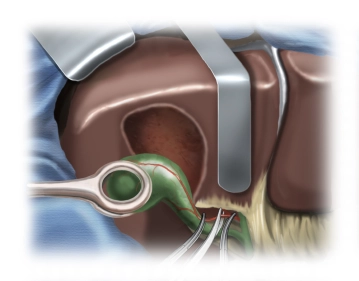
Following the skin incision, sharply take down the subcutaneous tissue to the anterior lamina of the rectus sheath. Open up the fascia and transversely transect the rectus abdominis by electrocautery. Bluntly running a Kocher guide probe under the rectus abdominis helps prevent thermal injuries to the posterior structures. Transect the external and internal oblique muscles and the transversus abdominis at the lateral part of the incision. Carefully open up the exposed posterior rectus sheath/transverse fascia together with the peritoneum, sparing the intraabdominal structures.
Note:
Pararectal incisions are obsolete.
The length of the incision depends on the patient’s individual situation.
Never transect along the costal arch because this will not leave enough tissue for proper wound closure.
In case of a markedly enlarged liver make the incision markedly more inferior.