Considering an incarceration rate of 30% with a lethality of up to 15%, there is no doubt about the indication for surgical treatment of ventral abdominal wall hernias. An exception are small umbilical hernias whose fascial gap is less than 0.5 cm and therefore have only a low risk of incarceration.
Hernia repair by direct suture is possible according to the guidelines of the European and American Hernia Society up to a hernia gap diameter of < 1 cm, provided there is no obesity (BMI > 30) and/or rectus diastasis.
EHS (European Hernia Society) and AHS (American Hernia Society) see the limit for the use of a mesh at > 1 cm. Only for defects of 0 - < 1 cm should a suture procedure be chosen with a margin of discretion for defects between 1 - 2 cm. Up to 4 cm, a preperitoneal mesh plasty is recommended, alternatively, minimally invasive sublay techniques (E/Milos, eTEP, TES) are also used, especially in the presence of rectus diastasis.
Round self-expanding meshes are obsolete because no broad parietalization, which is only possible laparoscopically, occurs. The reason is the anatomy of the plicae converging in the umbilicus, which prevent the unfolding of these meshes. The preperitoneal space is the actual optimal layer for umbilical meshes.
Presented in the article is the open preperitoneal, umbilical mesh plasty = PUMP-Repair.
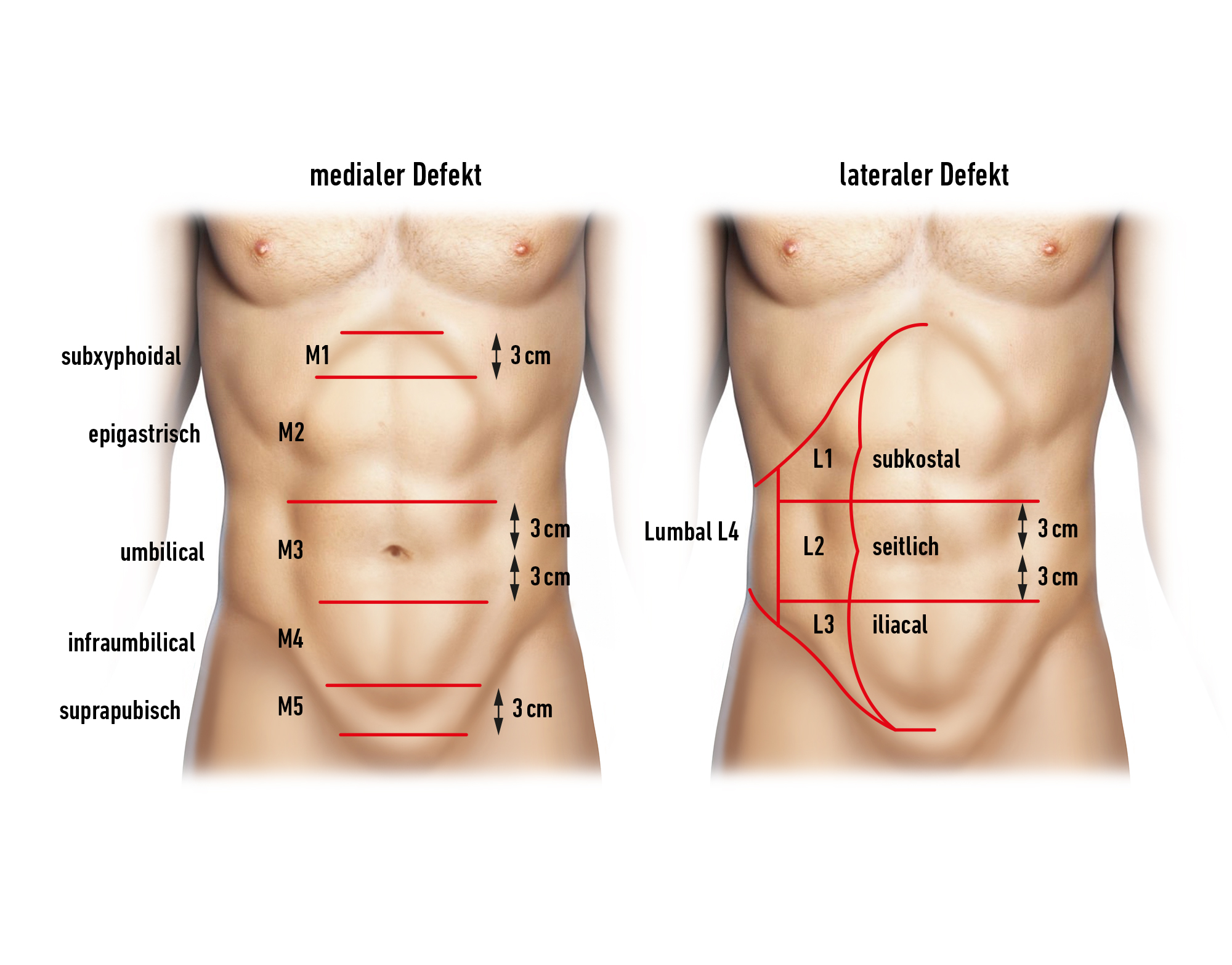
This is a preperitoneal mesh technique with defect closure after insertion of a mesh that should overlap the defect by 3 cm on all sides. Therefore, the peritoneum must be dissected from the abdominal wall all around 3 cm around the defect.
In the open repair of ventral hernias, the hernia orifice is basically only stretched, but not surgically enlarged. An enlargement of the hernia orifice would transform a primary hernia into an incisional one with a significantly higher recurrence rate.
In obesity, there are data with lower wound complication rates for lap IPOM compared to open procedures.
For defects > 4 cm, proceed as with incisional hernias.