With the patient in lithotomy position, perform a digital rectal examination followed by slow and careful dilation of the anal sphincter. Insert the Parks retractor
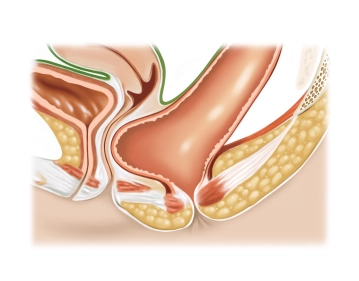
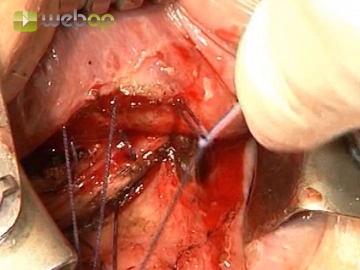
Injection into the anterior rectal mucosa, horizontal mucosal incision 5-8 mm proximal to the dentate line and careful excision of a longitudinally ovoid mucosal flap of up to 10 x 8 cm in size in cranial direction with diathermy while sparing the underlying muscle coat. Carry out the dissection in semicircular fashion, from 9 o'clock to 3 o'clock horizontally and vertically along the entire length of the rectocele.