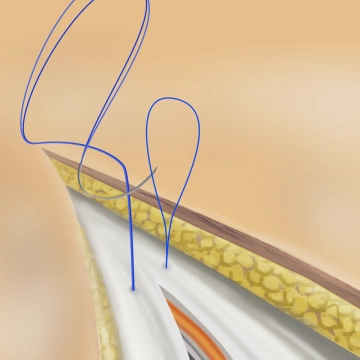
Hold the fascia with the surgical forceps and with a twisting motion place a stitch through the fascia 1 cm from the edge Grasp the anterior and posterior fascial laminae together.
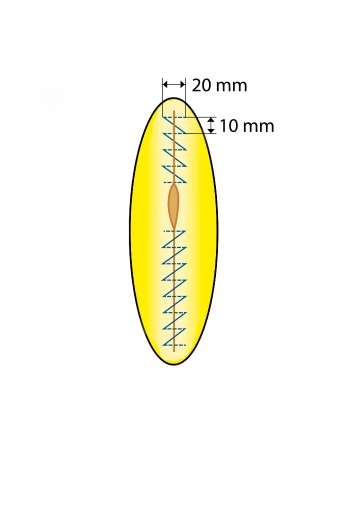
Place the first stitch about 1 cm craniad of the end of the wound to anchor the loop in the region of the fascia not incised. Start the V-shaped stitch from healthy tissue into the incision and from the incision back into healthy tissue on the contralateral side (outside in, inside out). Pull the needle through the loop and then continue in standard running technique. Suture the loop from the edge of the wound toward its middle. Space the sutures about 1 cm apart, resulting in a suture-to-wound length ratio of at least 4:1. Continue the superior row of sutures toward the midpoint of the incision.
Note: For fascial sutures, grasp only the aponeurosis, since muscle caught by the suture would become necrotic, resulting in loosening of the fascial closure. While the peritoneum does not have to be closed separately, it may be included in the suture. Avoid peritoneal bulging in the suture line.