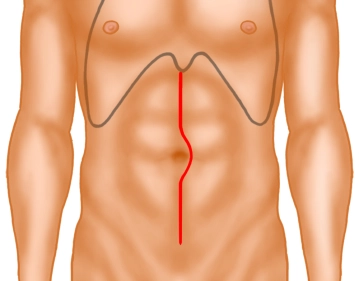
Opening of the abdominal cavity through a median laparotomy. It is very important to ensure that the skin incision is actually carried down to the symphysis, as otherwise access to the pelvis is significantly impeded. Afterwards, a covering, in this case a foil, is inserted and the abdominal walls are held aside by means of a retractor. Next, the intraoperative assessment of findings takes place (not shown).
-
Laparotomy and Exposure
-
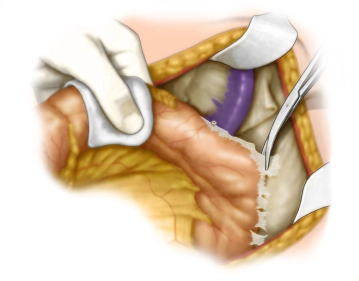
Mobilization of the left colon
![Mobilization of the left colon]()
Soundsettings The mobilization of the left flexure occurs alternately from aboral by dissecting the descending colon in an avascular layer in front of the left kidney and from oral by detaching the greater omentum from the colon up to about the middle of the transverse colon with opening of the omental bursa. Finally, the connections to the spleen and pancreas are released.
-
Management of the Inferior Mesenteric Vein
-
Management of the Inferior Mesenteric Artery
Soundsettings The inferior mesenteric artery is divided while sparing the superior hypogastric plexus approximately 1–2cm distal to its origin from the aorta, but proximal to the takeoff of the left colic artery, including the central lymph nodes. The central vascular stump is secured with a transfixing ligature.
Tip: Central ligation of the inferior mesenteric artery is not oncologically mandatory in rectal carcinoma. However, compared to selective ligation of the superior rectal artery while preserving the left colic artery, a tension-free anastomosis can be created more easily, which is why this approach is usually favored despite the potential disadvantages (poorer perfusion, damage to the preaortic nerves).
Note: A primary vessel division is a priori oncologically sensible, but an advantage has not been proven by studies.
-
Entering the Pelvis
Soundsettings After head-down positioning, preparation is first made from the right lateral side into the lesser pelvis by transecting the pelvic floor peritoneum at the peritoneal reflection fold. Then, entry is made into the mesorectal plane from the dorsal side with careful preservation of the nerves in the lesser pelvis. Finally, entry into the dorsal plane is made in a similar manner also on the left side, starting with an incision of the peritoneum at the lateral reflection.
Note: Already here, meticulous attention must be paid to the preservation of the mesorectum.
The next step is the complete detachment of the mesorectum from the presacral fascia and then furth
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$88.58/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$177.20 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.