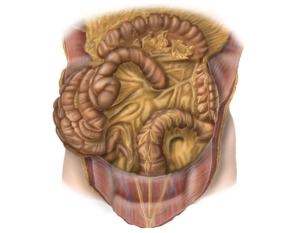
- Left colic flexure fixed to the diaphragm by the phrenicocolic ligament
- secondary retroperitoneal position of the descending colon
- Transition descending colon – sigmoid colon in the left iliac fossa
- intraperitoneal position of the sigmoid colon (→ sigmoid mesocolon)
- Transition sigmoid colon – rectum in front of the 2nd-3rd sacral vertebra
-
Descending Colon and Sigmoid Colon
![Descending Colon and Sigmoid Colon]()
-
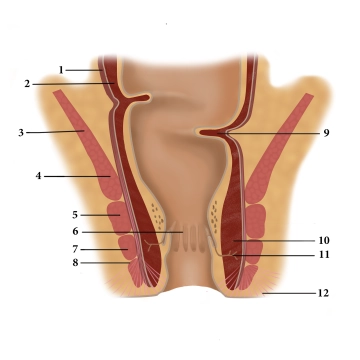
Rectum and Anal Canal
![Rectum and Anal Canal]()
(1) Tunica muscularis longitudinale, (2) Tunica muscularis circulare , (3) M. levator ani, (4) M. puborectalis, (5) M. sphincter ani profundus, (6) Columnae anales, (7) M. sphincter ani superficialis, (8) M. sphincter ani subcutaneus, (9) Kohlrausch fold, (10) M. sphinkter internus , (11) Proctodeal gland, (12) M. corrugator ani
Rectum
Functionally, the rectum represents a fecal reservoir that prevents continuous fecal discharge. It connects directly to the sigmoid colon and, like it, exhibits an S-shaped a/p and lateral curvature (Flexura sacralis, anorectalis and lateralis). Typically, the rectum is divided into three sections:
- Ampulla recti (main reservoir, ventral to the sacrum)
- Canalis analis (see below, closure region between the anorectal flexure and the skin opening)
- between 1 and 2, an unspecified section that emerges at a right angle from 1 and transitions at a right angle into 2. Here, typical folds (Kohlrausch folds) are found in the mucosa.
Adjacent structures of the rectum are dorsally the sacrum and coccyx, laterally next to the A. and V. iliaca int. the regional lymph nodes, the sacral plexus and parts of the autonomic nervous system, as well as ureters and adnexa. Ventrally, in the female organism, uterus and vagina, in the male, urinary bladder and prostate/seminal vesicles. Caudally, the pelvic floor is located.
Read here more about the histology of the rectum.
Anal Canal
Three muscles form the closure apparatus in the wall of the lower rectum:
- The internal anal sphincter represents a thickening of the last circularly running fibers of the smooth large intestine musculature and is innervated by the sympathetic nervous system.
- The levator ani muscle, on the other hand, is voluntarily innervated (sacral plexus) and the puborectalis muscle attached to the pubic bone is also attributed to it. It pulls as a large loop around the anal canal ventrally and thereby functionally kinks it.
- The external anal sphincter is also striated and suspended between the center of the perineal region (Centrum perinei) and the coccyx. It is voluntarily innervated by the pudendal nerve. Through its contraction, the anal canal is terminally closed.
The different innervation of the three closing muscles provides additional security against failures and resulting incontinence.
In the mucosa of the anal canal, numerous longitudinally running folds (Columnae anales) are found, which have dense arterial (!) plexuses with venous drainage. Upon contraction of the sphincter muscles, they fill up quickly and the mucosa swells, lies against each other, and thus provides a gas-tight closure. Hemorrhoids and venous thromboses are known vascular-related complications of this region.
Defecation occurs on the one hand through the relaxation of the closure mechanisms (initiated by the voluntary musculature, emptying of the corpora cavernosa) and on the other hand through active abdominal press and the peristalsis of the intestine.
-
Fascial Systems
- Parietal pelvic fascia covers pelvic wall with vessels, autonomic nerves and presacral venous/nerve plexus
- Above the anorectal junction meeting of the rectosacral fascia and the visceral pelvic fascia
- The visceral fascias include the fascia propria of the pelvic organs (enclose the mesorectum dorsally and laterally) and the ventrally located Denonvilliers' fascia
-
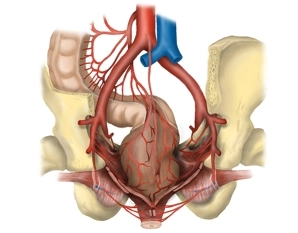
Vessels
![Vessels]()
- Anastomosis between the vascular territory of the superior mesenteric artery (A. colica media) and inferior mesenteric artery (A. colica sinistra) near the left colic flexure (arcade of Riolan).
- Supply of the left hemicolon, the sigmoid colon, and the upper rectum by the inferior mesenteric artery and its branches: A. colica sinistra, Aa. sigmoideae with the arcade of Drummond, A. rectalis superior.
- Supply of the upper third of the rectum via A. rectalis superior, which divides dorsally into two terminal branches, of the middle third from the A. rectalis media (paired, each as a branch of the A. iliaca interna) and of the lower third via A. rectalis inferior (paired, each as a branch of the A. pudenda interna from the A. iliaca interna). The Aa. rectales mediae run in the so-called lateral ligaments of the rectum and are transected during total mesorectal excision.
- Venous drainage of the left hemicolon via homonymous veins into the portal vein system.
- Venous drainage of the upper two thirds via the V. mesenterica inferior (portal vein system) and of the lower third via the drainage area of the V. cava inferior.
For all rectal segments along the course of the superior rectal artery and the inferior mesenteric
Activate now and continue learning straight away.
Single Access
Activation of this course for 3 days.
Most popular offer
webop - Savings Flex
Combine our learning modules flexibly and save up to 50%.
US$88.58/ yearly payment
general and visceral surgery
Unlock all courses in this module.
US$177.20 / yearly payment
Webop is committed to education. That's why we offer all our content at a fair student rate.