The reconstruction of the abdominal wall in complex incisional hernias or the presence of a laparostoma presents a particular challenge. A "loss of domain" represents the extreme form of a volume displacement of the intestines.
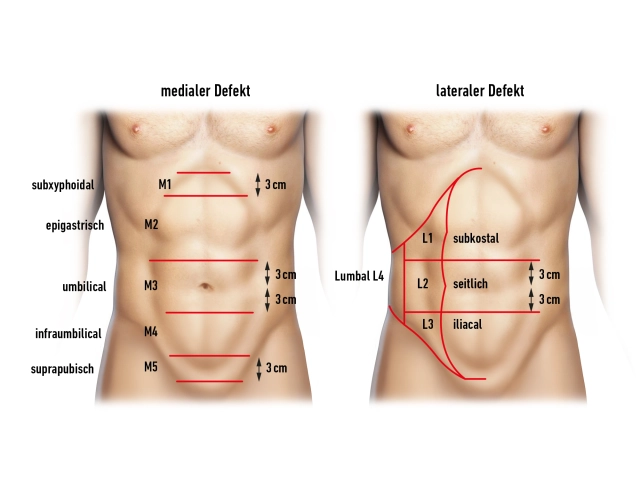
Complex hernias are considered abdominal wall hernias with defect widths of more than 10 cm, incisional hernia recurrence after mesh implantation (mesh edge herniation, mesh tear, mesh rupture), hernias after flap transfer (denervation, donor site defects), and multiple recurrences.
The abdominal wall defect after laparostoma represents a special situation. An abdominal wall closure has never occurred here. Complicating matters, there is no natural skin in the area of the abdominal wall defect, but rather a split-thickness skin graft. There is also no hernia sac helpful for reconstruction. The closure of the skin can present an additional problem.
In principle, the indication for repair of even a complex hernia is given. The patients lack ventral stabilizing elements of the trunk musculature. Patients with such unstable abdominal walls complain of postural problems with back pain. Physically demanding activities and sports are severely restricted to impossible. An intact ventral abdominal wall is of great importance for physiological processes such as breathing and defecation.
Furthermore, the abdominal wall defect and the extra-abdominal organ volume will continue to increase. The reconstruction of the abdominal wall is ultimately carried out to prevent increasing morbidity.
To achieve a fascial closure in the midline in these hernias, an abdominal wall component separation is usually required.
With the anterior component separation ("Ramirez") presented here, midline defects with a width of periumbilical up to 20 cm, epigastric up to 8 cm, and suprapubic up to 6 cm in diameter can be closed by separating parts of the lateral abdominal wall. The technique allows for a tension-free closure with a dynamically competent abdominal wall.
Due to the broad detachment of the subcutaneous tissue with the risk of destroying perforating vessels (blood supply to subcutaneous tissue and skin by the deep epigastric vessels) and the resulting high rate of wound healing disorders, hematomas, and seromas, this technique is now considered only a second-choice procedure. The posterior component separation, which leads to a release in the area of the M. transversus, is favored; additionally, the mesh bed can be expanded laterally, dorsally, and retrocostally.
The reconstruction according to Ramirez was described in the original work without mesh augmentation. The results in the literature favor the simultaneous implantation of a retromuscular mesh.
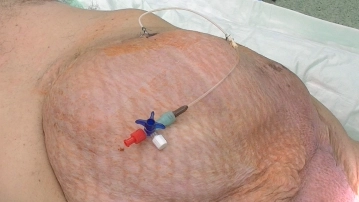
In the demonstrated case, as a special feature, in the absence of material for the closure of the peritoneum or the posterior rectus sheath, a defect bridging with the introduction of a biological mesh is shown. Alternatively, an IPOM-capable synthetic mesh can also be used. The advantage of a biological mesh is the possibility of application in an infected surgical field, better stretchability, and the natural remodeling into the body's own tissue.
The introduction of botulinum toxin for the relaxation of the lateral abdominal wall musculature has significantly reduced the necessity of component separation in midline hernias.