According to the guidelines of the EHS and AHS, the open sublay technique is an option for the treatment of primary and secondary abdominal wall hernias with defects between 4 and 10 cm.
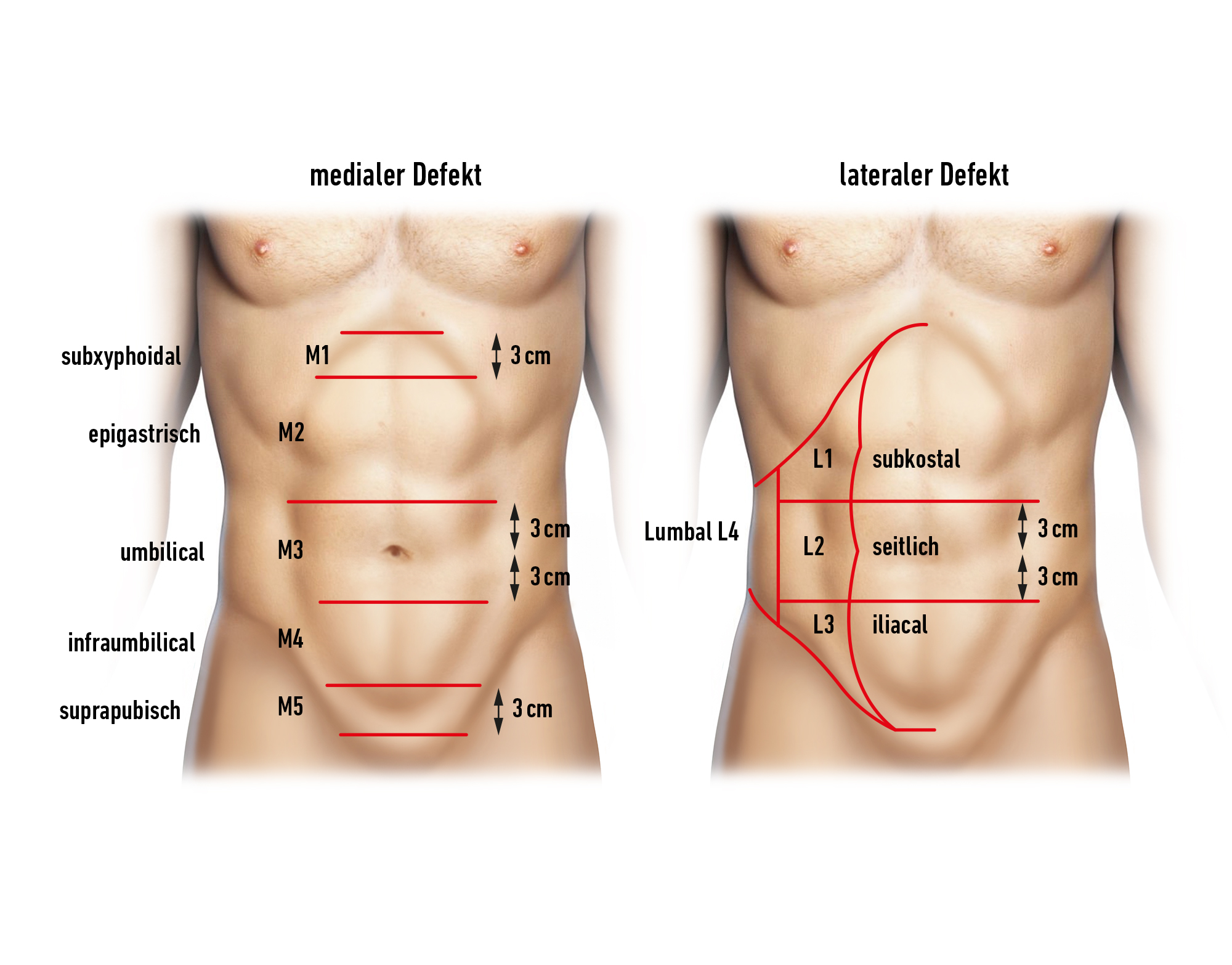
For retromuscular mesh positioning behind the M. rectus abdominis, this technique is particularly suitable for midline defects.
In the incarceration situation, depending on the degree of contamination, treatment with a synthetic mesh is indicated only with great caution.
Due to the evidence of the retromuscular layer as the optimal mesh placement, there has been a renaissance of the open sublay procedure in incisional hernia surgery in recent years.
The sublay technique describes a retromuscular preperitoneal position of the mesh, which ideally includes a midline reconstruction with closure of the fascia over the mesh. This achieves a good mesh counterbearing, with the intra-abdominal pressure resting on the mesh as the strongest component of the closure and supporting its fixation.
In principle, the indication for repair of an abdominal wall hernia is always given, as the hernia gap and extra-abdominal organ volume will usually continue to increase. In larger defects, ventral stabilizing elements of the trunk musculature are missing. Physically demanding activities and sports can be severely restricted to impossible.
The exception is only the incidental finding in the context of cross-sectional imaging for other reasons. In the absence of symptoms, there is not necessarily an indication for surgery here.