According to the guidelines of the EHS and AHS, the laparoscopic IPOM technique is recommended for larger primary and secondary abdominal wall hernias and in patients with an increased risk of wound complications. This particularly concerns patients with obesity (BMI >_ 30) and patients with a defect size of over 4 cm. However, the defect should not exceed a size of 8 - 10 cm.
The laparoscopic intraperitoneal mesh implantation currently represents the most common endoscopic, minimally invasive technique for the treatment of abdominal hernias worldwide. In Germany, however, there is a decline in this method due to fear of adhesiogenesis with the formation of prosthetic-intestinal fistulas despite improved meshes regarding their coating. Other reasons include an increased rate of acute and chronic postoperative pain, presumably because the method is expensive. Nevertheless, it is an important alternative technique.
Secondary abdominal wall hernias:
Incisional hernia is the most common complication after laparotomy with a prevalence between 3 and 40% regardless of the abdominal wall closure chosen.
Risk factors for the development of incisional hernias:
BMI >_ 25, male gender, recurrent incision, malignant disease, wound contamination, open surgery, COPD, positive family history.
When determining the indication, the previous intervention should be at least 6 months ago.
Closure of the hernia defect:
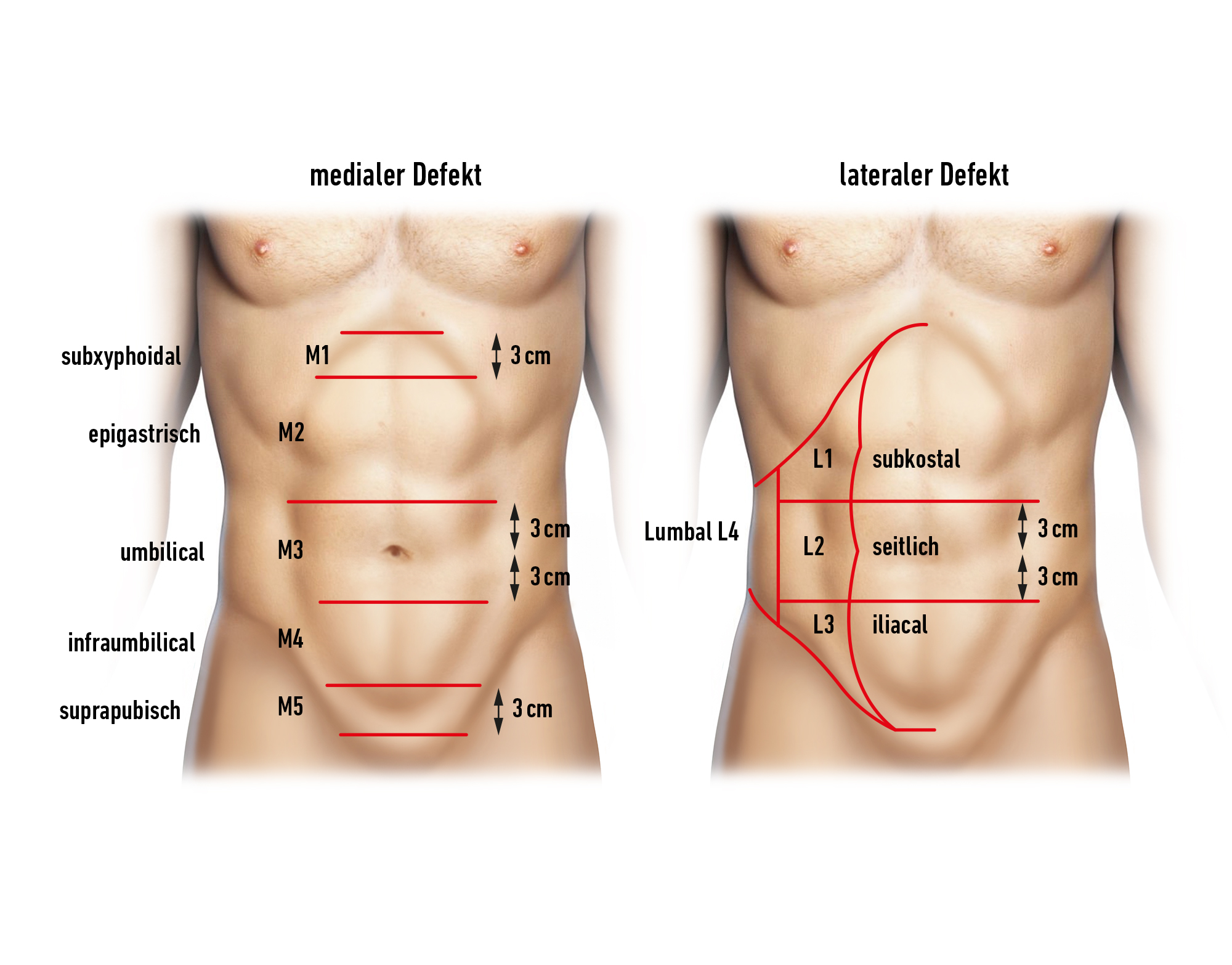
There are studies that recommend an additional closure of the hernia defect in IPOM to reduce the rate of recurrences, seroma formation, and pseudo-recurrences. In the case of a small defect (< 3cm), a direct closure of the defect is used, and for larger defects, a so-called LIRA (intracorporeal rectus aponeuroplasty) with a knotless suture is applied. In a recent study (Pizza F et al 2023), the superiority of a hernia defect closure could not be confirmed.