Inguinal region from the inside: (1) Inferior epigastric artery and vein, (2) medial = direct inguinal hernia orifice, (3) femoral hernia orifice, (4) pectineal ligament (Cooper), (5) ductus deferens, (6) external iliac artery and vein, (7) testicular artery and vein, (8) iliopubic tract, (9) lateral = indirect inguinal hernia orifice
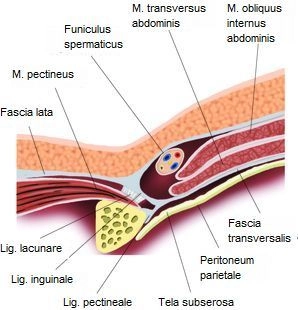
The inguinal region (transition between the anterior abdominal wall and lower extremity) has several weak points through which a hernial sac with or without contents can protrude through the abdominal wall (women are more prone to femoral hernias, men to inguinal hernias). Below the inguinal ligament, the inguinal canal is divided into two compartments by a separation of the inguinal ligament (iliopectineal arch): the vascular lacuna and the muscular lacuna.
- Vascular Lacuna
Located next to the pubic bone, it serves as the passageway for the external iliac artery and vein (→ femoral artery and vein, arrangement: artery lateral to the vein). Additionally, the femoral branch of the genitofemoral nerve passes through it laterally, and the deep inguinal lymph nodes (Rosenmüller) are found caudally medial within it. The vascular lacuna represents the internal hernia gap for femoral hernias (through the femoral septum next to the femoral vein).
- Muscular Lacuna
Located lateral to the vascular lacuna, it serves as the passageway for the psoas major muscle and iliacus muscle (together = iliopsoas muscle) as well as the femoral nerve and lateral cutaneous femoral nerve (cranially).